- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(1); 2021 > Article
-
Original ArticleGuideline/Fact Sheet Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status
-
Chan-Hee Jung1
 , Jang Won Son2, Shinae Kang3, Won Jun Kim4, Hun-Sung Kim5, Hae Soon Kim6, Mihae Seo7, Hye-Jung Shin8, Seong-Su Lee2, Su Jin Jeong9, Yongin Cho10, Seung Jin Han11, Hyang Mi Jang12, Mira Rho13, Shinbi Lee14, Mihyun Koo15, Been Yoo16, Jung-Wha Moon17, Hye Young Lee18, Jae-Seung Yun19, Sun Young Kim20, Sung Rae Kim2, In-Kyung Jeong21, Ji-Oh Mok1
, Jang Won Son2, Shinae Kang3, Won Jun Kim4, Hun-Sung Kim5, Hae Soon Kim6, Mihae Seo7, Hye-Jung Shin8, Seong-Su Lee2, Su Jin Jeong9, Yongin Cho10, Seung Jin Han11, Hyang Mi Jang12, Mira Rho13, Shinbi Lee14, Mihyun Koo15, Been Yoo16, Jung-Wha Moon17, Hye Young Lee18, Jae-Seung Yun19, Sun Young Kim20, Sung Rae Kim2, In-Kyung Jeong21, Ji-Oh Mok1 , Kun Ho Yoon22
, Kun Ho Yoon22 -
Diabetes & Metabolism Journal 2021;45(1):1-10.
DOI: https://doi.org/10.4093/dmj.2020.0254
Published online: January 13, 2021
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
10Department of Endocrinology and Metabolism, Inha University School of Medicine, Incheon, Korea
11Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
12Department of Nursing, Gangnam Severance Hospital, Yonsei University, Seoul, Korea
13Department of Nutrition, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea
14Department of Clinical Nutrition, Korea University Anam Hospital, Seoul, Korea
15Department of Social Work, Samsung Medical Center, Seoul, Korea
16Department of Social Work, Kyung Hee University Hospital at Gangdong, Seoul, Korea
17Department of Sports Medical Center, Inje University Ilsan Paik Hospital, Goyang, Korea
18Sport Health Medicine Center, Asan Medical Center, Seoul, Korea
19Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
2Division of Endocrinology and Metabolism, Department of Internal Medicine, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
20Department of Nursing, Samsung Medical Center, Seoul, Korea
21Division of Endocrinology and Metabolism, Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea
22Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, the Catholic University of Korea, Seoul, Korea
3Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
4Department of Endocrinology and Metabolism, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
5Department of Medical Informatics, College of Medicine, The Catholic University of Korea, Seoul, Korea
6Department of Pediatrics, Ewha Womans University School of Medicine, Seoul, Korea
7Department of Endocrinology and Metabolism, Soonchunhyang University Gumi Hospital, Soonchunhyang University College of Medicine, Gumi, Korea
8Department of Pediatrics, National Medical Center, Seoul, Korea
9Department of Endocrinology and Metabolism, Sejong General Hospital, Bucheon, Korea
-
Corresponding author: Ji-Oh Mok
 Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, 170 Jomaru-ro, Wonmi-gu, Bucheon 14584, Korea E-mail: hanna@schmc.ac.kr
Division of Endocrinology and Metabolism, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, 170 Jomaru-ro, Wonmi-gu, Bucheon 14584, Korea E-mail: hanna@schmc.ac.kr
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- This study aimed to investigate the recent prevalence, management, and comorbidities of diabetes among Korean adults aged ≥30 years by analyzing nationally representative data.
-
Methods
- This study used data from the Korea National Health and Nutrition Examination Survey from 2016 to 2018, and the percentage and total number of people ≥30 years of age with diabetes and impaired fasting glucose (IFG) were estimated.
-
Results
- In 2018, 13.8% of Korean adults aged ≥30 years had diabetes, and adults aged ≥65 years showed a prevalence rate of 28%. The prevalence of IFG was 26.9% in adults aged ≥30 years. From 2016 to 2018, 35% of the subjects with diabetes were not aware of their condition. Regarding comorbidities, 53.2% and 61.3% were obese and hypertensive, respectively, and 72% had hypercholesterolemia as defined by low-density lipoprotein cholesterol (LDL-C) ≥100 mg/dL in people with diabetes. Of the subjects with diabetes, 43.7% had both hypertension and hypercholesterolemia. With regard to glycemic control, only 28.3% reached the target level of <6.5%. Moreover, only 11.5% of subjects with diabetes met all three targets of glycosylated hemoglobin, blood pressure, and LDL-C. The percentage of energy intake from carbohydrates was higher in diabetes patients than in those without diabetes, while that from protein and fat was lower in subjects with diabetes.
-
Conclusion
- The high prevalence and low control rate of diabetes and its comorbidities in Korean adults were confirmed. More stringent efforts are needed to improve the comprehensive management of diabetes to reduce diabetes-related morbidity and mortality.
- Over the past few decades, the prevalence of diabetes has steadily increased [1-3]. Globally, 425 million people, representing 8.8% of the global adult population (20 to 79 years) in 2017 and 463 million (9.3%) in 2019, are estimated to be living with diabetes according to the International Diabetes Federation (IDF) Diabetes Atlas [1]. The global prevalence of diabetes has nearly doubled since 1980, rising from 4.7% to 9.3% in the adult population [2,3]. In addition, of the 463 million people living with diabetes, half (50.1%) are unaware of their condition [1].
- A high burden of diabetes complications as well as diabetes itself have a significant impact on population health. Diabetes was the eighth leading cause of death among both sexes and the fifth leading cause of death in women in 2012 globally [4]. In Korea, diabetes was the sixth leading cause of death among both sexes [5]. In particular, age-standardized mortality due to diabetes was higher in Korea than in other countries that are part of the Organisation for Economic Co-operation and Development (OECD) [6]. Therefore, there is an urgent need to implement interventions that prevent diabetes, enhance its early detection, and promote lifestyle modifications and aggressive medical treatment to prevent or delay complications. In addition, valid and consistent estimates of diabetes prevalence are needed to evaluate the effect of interventions, compare trends over time, and estimate reaching diabetes targets.
- Since 2012, the Korean Diabetes Association (KDA) has published Diabetes Fact Sheets (DFS) based on the Korea National Health and Nutrition Examination Survey (KNHANES), a nationwide survey conducted by the Korean Centers for Disease Control and Prevention (KCDC). The purpose of this DFS is to provide national representative statistics on the prevalence and numbers of diabetes and impaired fasting glucose (IFG) and the management status of diabetes and its comorbidities in Korea. The objective of this study was to investigate the prevalence, total number, management, and comorbidities of diabetes among Korean adults ≥30 years by analyzing nationally representative KNHANES data. In addition, energy intake and percentage of energy intake from each macronutrient were investigated among those with diabetes, previously diagnosed diabetes, and those without diabetes.
INTRODUCTION
- Study population
- This study analyzed data from KNHANES VII (2016 to 2018). KNHANES is a population-based cross-sectional survey that employs a rolling sampling design involving a stratified, multistage, probability cluster survey of a representative sample of the Korean population [7,8]. It consists of three surveys: a health interview survey, a health examination survey, and a nutrition survey. The total number of subjects ≥30 years of age with diabetes and IFG were determined based on the National Population Census in 2018. We constructed two datasets from KNHANES as follows: (1) KNHANES 2018 and (2) KNHANES 2016 to 2018 (merged 3 years of data). Data from KNHANES 2018 were used to calculate the prevalence of diabetes and IFG. Data for KNHANES 2016 to 2018 (merged 3 years of data) were used to identify the management status of diabetes and comorbidities in diabetes and energy intake.
- Informed consent was obtained during the process of KNHANES, and this manuscript was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital (IRB No. 2020-05-001).
- Biochemical measurements
- After overnight fasting, fasting plasma glucose (FPG), total cholesterol (TC), high-density lipoprotein cholesterol (HDLC), and triglyceride (TG) levels were measured using a Hitachi Autonomic Analyzer 7600 (Hitachi, Tokyo, Japan). Low-density lipoprotein cholesterol (LDL-C) was measured by direct assay for persons with TG >200 mg/dL (Hitachi Automatic Analyzer 7600). Thus, we used either directly measured or calculated LDL-C according to the Friedewald formula: LDL-C=TC–HDL-C–(TG/5) [9]. Glycosylated hemoglobin (HbA1c) levels were measured using high-performance liquid chromatography (HLC-723G7; Tosoh, Tokyo, Japan).
- Definitions of IFG, diabetes, and its related comorbidities
- The diagnosis of diabetes was based on FPG ≥126 mg/dL, current use of anti-diabetic medication(s), a previous history of diabetes, or HbA1c ≥6.5% [10]. IFG was defined by FPG in the range of 100 to 125 mg/dL among those without diabetes [10]. The glycemic control rate in diabetes was defined as the rate of people with HbA1c <6.5% among people with diabetes (%). Overweight was defined as a body mass index (BMI; weight in kilograms divided by the square of height in meters) ≥23.0 kg/m2, and obesity was defined as a BMI ≥25.0 kg/m2 [11]. Abdominal obesity was defined as waist circumference ≥90 cm in men and ≥85 cm in women. Hypertension was defined as systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg and/or current use of antihypertensive medications. Control of hypertension was defined as SBP and DBP <140/85 mm Hg according to the KDA clinical practice guideline for Diabetes 2019 [12]. Hypercholesterolemia was defined as LDL-C ≥100 mg/dL or current use of lipid-lowering medication(s), and control of hypercholesterolemia was defined as LDL-C <100 mg/dL [12,13]. The awareness rate was defined as the rate of people diagnosed with diabetes by a doctor among people with diabetes (%). The treatment rate was defined as the rate of people treated with antidiabetic drugs among people with diabetes (%). The definitions of health behaviors are as follows: current smoking: smoked at least five packs of cigarettes (100 cigarettes) during the lifetime; high-risk drinking: ≥7 glasses in men or ≥5 glasses in women on the same occasion on each of 2 or more days a week; regular walking exercise: ≥5 days/week and for ≥30 minutes/activity.
- The daily food and energy intake were measured using a single day 24-hour dietary recall and semiquantitative food frequency questionnaire method [8]. For estimation of nutrient intake, the 2015 Dietary Reference Intake for Koreans was used [14]. Excessive energy intake was defined as the condition wherein the percentage of energy intake was greater than 125% of the estimated energy requirement recommended by the Korean Dietary Reference Intake [14]. The percentage of energy intake from carbohydrate, protein, and fat was calculated using the following methods: the percentage of energy intake from carbohydrate=(g of carbohydrate intake×4)/[(g of carbohydrate intake×4)+(g of protein intake ×4)]+(g of fat intake×9)]×100; the percentage of energy intake from protein=(g of protein intake×4)/[(g of protein intake×4)+(g of carbohydrate intake× 4)+(g of fat intake×9)]×100; the percentage of energy intake from fat=(g of fat intake×9)/[(g of fat intake×9)+(g of carbohydrate intake×4)+(g of protein intake×4)]×100.
METHODS
- Prevalence of diabetes and IFG
- Table 1 shows the prevalence of diabetes and IFG in 2018. Among Korean adults aged ≥30 years in 2018, the prevalence of diabetes was 13.8% (4.94 million). The prevalence of diabetes among Korean adults aged ≥65 years was 27.6%. There were differences in diabetes prevalence by sex, age group, and household income. The prevalence of diabetes in men was higher than that in women (15.9% vs. 11.8%). The prevalence of diabetes increased with age in both sexes. The prevalence exceeded 10% in their forties for men, while for women, it exceeded 10% in their 50s. In the group aged 40 to 49 years, the prevalence of diabetes was 3.7 times higher in men than in women (13% vs. 3.5%). However, in individuals aged 70 years and older, diabetes was more prevalent in women than in men (29.4% vs. 28.8%). By household income quintile, the prevalence in the lowest household income quintile was 14.4%, while that in the highest quintile was 8.6%.
- The prevalence of IFG in Korean adults aged ≥30 years in 2018 was 26.9% (9.48 million). IFG was more prevalent in men than in women (32% vs. 22%).
- Current status of managing diabetes
- From 2016 to 2018, only 65% of adults with diabetes were aware of their condition, and 60.1% were in treatment (oral hypoglycemic agent, 56%; insulin therapy, 4.1%) (Table 2). Most adults with previously diagnosed diabetes were being treated with oral hypoglycemic agents (86.1%), while 6.4% were treated with insulin with or without an oral hypoglycemic agent; 6.9% were not receiving any treatment for their disease (Supplementary Fig. 1). The glycemic control rate among people with diabetes was 28.3% for a target goal of HbA1c <6.5% (Supplementary Fig. 2). Of people with diabetes, 19.1% had HbA1c above 8.0%. According to the target level of the KDA treatment guidelines, 28.3% of people with diabetes achieved HbA1c <6.5%, 54.4% achieved blood pressure (BP) <140/85 mm Hg, and 53.3% achieved LDL-C <100 mg/dL.
- Comorbidities in adults with diabetes and health behaviors
- From 2016 to 2018, the prevalence of obesity and abdominal obesity in adults with diabetes was 53.2% (50.9% in men and 56.0% in women) and 54% (50.7% in men and 58.2% in women), respectively (Fig. 1). When obesity was categorized as class I to III, obesity class I (BMI 25.0 to 29.9 kg/m2) accounted for 41.5% of diabetes, obesity class II (BMI 30.0 to 34.9 kg/m2) accounted for 10.1%, and obesity class III (BMI ≥35 kg/m2) accounted for 1.6%. Morbid obesity of class II and III was 11.7% in adults with diabetes. In addition, the estimated prevalence and control rate of comorbidities are presented in Table 3. The prevalence of hypertension in adults with diabetes was 61.3%. Only 54.4% of adults with diabetes were controlled to the target level of BP. Regarding the prevalence of hypercholesterolemia, the prevalence was 72% when based on LDL-C >100 mg/dL or antilipidemic agents, and the control rate of hypercholesterolemia was 53.5%.
- Regarding health behaviors, 21% were current smokers (men 34.9% vs. women 3.7%), 23.1% were high-risk drinkers (men 30.7% vs. women 6.8%), and 35.7% were walking regularly (men 36.4% vs. women 34.9%) among adults 30 years of age with diabetes (Supplementary Table 1).
- Prevalence of both hypertension and hypercholesterolemia in adults with diabetes
- The prevalence of both hypertension and hypercholesterolemia was 43.7% (39.4% in men, 49% in women) in adults ≥30 years of age with diabetes and 51.4% (43.8% in men, 57.2% in women) in adults ≥65 years (Table 3). Only 11.5% of subjects with diabetes met all three target levels (HbA1c <6.5%, BP <140/85 mm Hg, and LDL-C <100 mg/dL).
- Dietary intake in adults with diabetes from 2016 to 2018
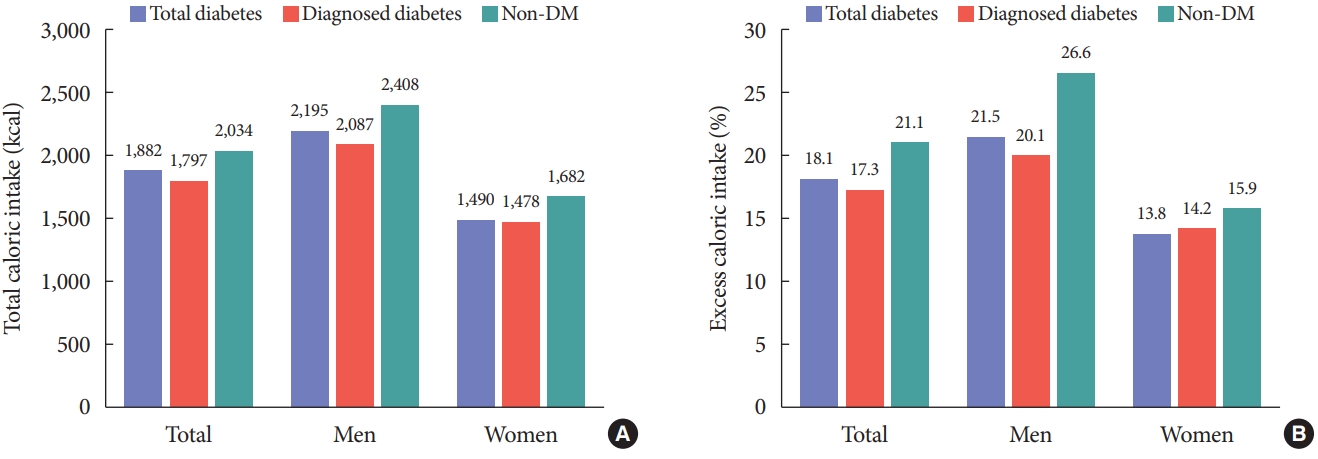
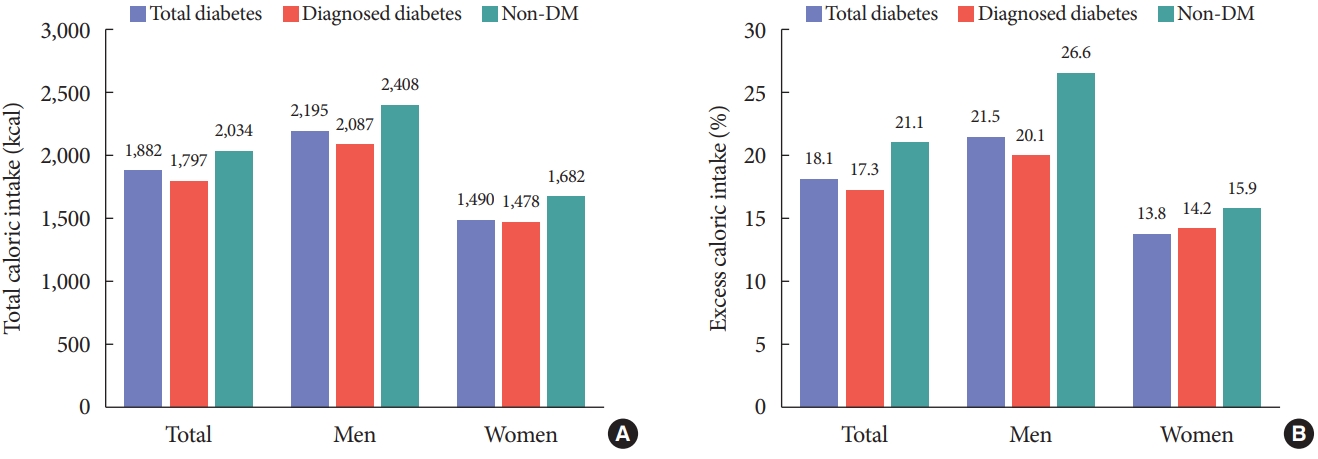
- Total daily energy intake, excess energy intake, and percentage of energy intake from macronutrients were evaluated among subjects with diabetes, with previously diagnosed diabetes, and those without diabetes (Table 4 and Fig. 2). Total energy intake and excess energy intake were higher in subjects without diabetes than in those with diabetes (total or previously diagnosed) (Fig. 2). The percentage of energy intake from carbohydrates was high in the diabetes group compared to those without diabetes (68.3% in diabetes, 69.9% in diagnosed diabetes, and 64.7% in without diabetes) (Table 4). On the other hand, the percentage of energy intake from protein and fat was lower in subjects with diabetes than in those without diabetes (for protein: 14.5% in diabetes, 14.1% in diagnosed diabetes, and 15.2% in without diabetes, respectively; for fat: 17.1% in diabetes, 16.0% in diagnosed diabetes, and 20.1% in without diabetes, respectively) (Table 4).
RESULTS
- In 2018, the prevalence and estimated number of diabetes cases among adults ≥30 years were 13.8% and 4.94 million, respectively. The prevalence of diabetes steadily increased over 17 years from 2001 (8.6%) to 2018 (13.8%) in adults ≥30 years of age in a nationally representative sample of Koreans [15-18]. HbA1c has been included in the diagnostic criteria for the diagnosis of diabetes since KNHANES 2011. More specifically HbA1c increased from 12.4% in 2011 to 14.5% in 2013 and then decreased slightly to 13.0% and 11.4% in 2014 and 2015, respectively [17,19]. Then, it increased again to 14.4% in 2016 and stayed at approximately 14% [18,20]. In addition, the estimated number of people with diabetes (30 to 79 years) has increased by 54% during the past 8 years, from 3.20 million in 2010 to 4.94 million in 2018 [18,21].
- The global age-standardized diabetes prevalence has grown from 4.7% in 1980 to 8.5% in 2014, and this rise in prevalence has been compounded by population growth, aging, and increasing overweight or obesity, nearly quadrupling the number of adults with diabetes over these 35 years [3]. In the IDF Atlas, the global prevalence of diabetes in adults aged 20 to 79 years representing 138 countries was estimated to be 8.8% in 2017 and 9.3% in 2019 and is predicted to rise to 10.9% in 2045 [1]. Although it is difficult to fully compare differences in diabetes prevalence worldwide due to different data sources, study sample sizes, ages of the study population, and heterogeneity of definitions of diabetes, it is clear that the prevalence of diabetes has been steadily increasing for the past 3 decades globally.
- Prevalence can be affected by the mortality and incidence of diabetes [22]. The prevalence can rise by improving the survival of people with diabetes and aging but can also decrease by decreasing or stabilizing the incidence. In Korea, the prevalence of diabetes has mainly increased due to population aging and increasing obesity [23,24]. Recently, in terms of incidence, some countries, including Korea, have shown decreasing or stable incidences of diabetes for several possible reasons [22]. It might be starting to benefit from prevention activities of type 2 diabetes mellitus (T2DM) and reductions in the pool of undiagnosed diabetes through increased uptake of the national health screening program. Based on the reported DFS thus far, the trend of prevalence during the past 7 years in Korea appears stable at a high rather than substantial rise.
- Consistent with the results of previous DFS 2016 and 2018, DFS 2020 also showed that the prevalence of diabetes increased with age in both sexes [18-20]. The prevalence of diabetes over the age of 65 was 27.6%, which was twice the prevalence of diabetes over the age of 30 (13.8%). Consistent with previous DFS and other countries, the prevalence of diabetes showed variations according to sex; that is, it was higher among men than women [18,19,25]. DFS 2020 also showed that lower family income level was associated with higher prevalence of diabetes in both sexes. The burden of diabetes has increased at a greater rate in low- and middle-income countries than in high-income countries globally [3].
- In addition, the prevalence and estimated number of IFGs were 26.9% and 9.48 million in adults aged ≥30 years and 29.6% and 2.17 million in adults aged ≥65 years, respectively. The estimated number of IFGs in this group was already 1.3 million. The prevalence of IFG gradually increased from 24.8% in DFS 2016 to 25.3% in DFS 2018 and to 26.9% in DFS 2020. We investigated the distribution of IFG prevalence according to sex and age. A higher prevalence of IFG was observed in men than in women at all ages. A drastic increase in the prevalence of IFG was observed among men aged 30 and 40 years and then decreased among elderly individuals above 60 years, whereas the prevalence among women showed a continuous increase with age. The estimated number of IFGs was reversed in both men and women for the elderly population aged above 70 years. Prevalence estimates of IFG reported in the literature vary greatly due to the diagnostic criteria used, the screening test, and characteristics of the study population [26-28]. A large meta-analysis of studies that reported prevalences in Caucasian and Asian cohorts estimated the IFG prevalence to be 53.1% [27]. In another meta-analysis, the mean overall prevalence of IFG in Europe was 8.4% (7.1 to 9.9) [28]. The prevalence of IFG is clearly increasing rapidly in all parts of the world. Because of the increasing risks of T2DM and cardiovascular disease (CVD) in prediabetic (IFG, impaired glucose tolerance) subjects and the possible reversibility of IFG, contrary to the irreversibility of diabetes, IFG has received increasingly widespread attention [29]. For the young age group, long-term exposure to IFG risks can lead to the early development of diabetes and vascular complications. Therefore, early identification of people with IFG and preventive lifestyle modifications should be strongly recommended.
- Early intensive and continuous glucose control in people with diabetes can delay progression to microvascular and macrovascular complications. However, the effectiveness of these interventions at the population level has been unsatisfactory because considerable people with diabetes remain undiagnosed, and adherence to treatment may be low in the general population. In this study, the awareness and treatment of diabetes were 65% and 60.5%, respectively. Despite the improvements in screening and health promotion, 35% of the people with diabetes were unaware of their condition. In addition, 39.5% did not take treatment with glucose-lowering agents or modify their lifestyle. Nonetheless, the awareness and treatment proportion in this study were higher than those found in 2013 to 2016 (62.5% and 56.7%, respectively) and those found in China and Switzerland [18,30,31].
- Regarding glycemic control, the rate of good glycemic control (HbA1c <6.5%) in people with diabetes rose steadily from 24.8% in 2013–2014 to 25.1% in 2013–2016 to 28.3% in 2016–2018 [18,19]. The control rates of HbA1c <7.0% were 43.3%, 52.6%, and 56.9% in 2013–2014, 2013–2016, and 2016–2018, respectively [18,19]. In particular, the poor control rate (defined as HbA1c ≥9.0%) decreased steadily from 15.5% in 2013–2014 to 10.8% in 2013–2016 to 9.6% in 2016–2018 [18, 19]. Although the rate of good glycemic control of HbA1c <6.5% has increased steadily over the past 7 years, it is still as low as 30%.
- Regarding health behaviors, the rate of current smoking decreased from 27.4% in DFS 2016 to 24.1% in DFS 2018 and to 21.1% in DFS 2020, but the rate of high-risk alcohol drinking increased from 21.9% in DFS 2016 to 23.1% in DFS 2020. The rate of regular walking did not improve (37.9% in DFS 2016, 36.0% in DFS 2018, and 35.7% in DFS 2020). Large reductions in smoking rates occurred in the 1970s and 1980s, followed by gradual reductions thereafter [32]. Korea is no exception. According to the study by Park [33] investigating adherence to dietary recommendations between diagnosed and undiagnosed subjects with T2DM using 1998 to 2012 KNHANES, adherence to moderate alcohol drinking habits decreased over time, as was observed in the current DFS. In the present study, high-risk drinking was defined as ≥7 drinks/day in men, ≥5 drinks/day in women, and 2 times/week, whereas moderate alcohol consumption was defined as ≤1–2 drinks/day in Park’s study [33]. Although the definition of alcohol consumption was not identical between the two studies, the two studies all indicated decreasing trends in healthy alcohol consumption habits.
- Adults with diabetes continue to have a two to three times higher rates of CVD than adults without diabetes [34]. An increased prevalence of the comorbid conditions obesity, hypertension, and dyslipidemia, along with poor rates of glucose control, may potentiate CVD risk. Therefore, intense efforts for the prevention and proper management of diabetes and comorbid diseases are required.
- The prevalence of obesity steadily increased from 44.4% in 2011 to 48.6% in 2013–2014 to 50.4% in 2013–2016 and to 53.2% in 2016–2018 [18,19,24]. The rate of normal BMI was only 23.3% in this study. There has been little success in preventing and combating obesity despite global efforts and campaigns.
- The prevalence of hypertension in diabetes increased (54.6% in 2011, 54.7% in 2013–2014, 55.3% in 2013–2016, and 61.3% in 2016–2018). However, the control rate of hypertension was improved compared to KNHANES in 2011 (25.2% in new DM, 39.9% in known DM), whereas it showed no improvement thereafter (69.1% in 2013–2014, 68.4% in 2013–2016, and 67.9% in 2016–2018) [35]. The prevalence of hypercholesterolemia in this study was much higher than that of previous reports (72% vs. 31.6% in 2013–2014 and 34.9% in 2013–2016). This was largely caused by differences in the definition of hypercholesterolemia. Previous DFS defined hypercholesterolemia based on TC ≥240 mg/dL, whereas DFS 2020 defined hypercholesterolemia as LDL-C ≥100 mg/dL. In this study, when it was defined based on TC ≥240 mg/dL, the prevalence was 42.4% (37.1% in men, 49.1% in women, data not shown). Therefore, we cannot directly compare the differences in the prevalence of hypercholesterolemia between studies. The control rate of hypercholesterolemia as LDL-C <100 mg/dL increased somewhat from 49.8% in 2013–2016 to 55.3% in this study. In addition, nearly half of people with diabetes had both hypertension and hypercholesterolemia (43.7% in adults ≥30 years and 51.4% in adults ≥65 years).
- The comprehensive management of diabetes through achievement of ABC clinical targets (A, HbA1c <6.5%; B, BP <140/85 mm Hg; C, LDL-C <100 mg/dL) is important to prevent and delay vascular complications. However, only 11.5% of subjects achieved all three ABC targets in this study. Although all target achievement rates were still low, they showed increasing trends (9.4% in 2013–2014, 8.4% in 2013–2016, and 11.5% in 2016–2018).
- In the present fact sheet, we investigated the total energy intake, excess energy intake, and percentage of energy intake from each macronutrient among people with diabetes, with previously diagnosed diabetes, and those without diabetes. Less energy, protein, and fat intake and more carbohydrate intake were shown in people with diabetes than in people without diabetes. Although there is no ideal percentage of macronutrients or eating patterns that can apply to all people with diabetes, low carbohydrate and lower caloric intake have been a focus in diabetes [36]. In particular, Koreans traditionally have a high carbohydrate eating pattern; therefore, they have been recommended to eat fewer carbohydrates [37]. Relatively, modification of protein intake has been less of a focus, although low protein intake in Korea has been previously reported [37]. Regarding fat, people with diabetes may have a tendency and make an effort to eat less fat to control diabetesassociated comorbidities, such as obesity and hypercholesterolemia. Lee et al. [37] evaluated food patterns of a high-carbohydrate diet among the Korean general population aged ≥20 years using data from the 2013 to 2015 KNHANES. Fifty-eight percent of men and 60% of women exceeded the recommended range of carbohydrate intake. A higher carbohydrate diet was associated with intake of low energy and saturated fats, with more grains and fruit but little consumption of proteincontaining foods, such as meat, fish, eggs, beans, and milk. Energy intake decreased across the carbohydrate groups. They found a positive association of dietary carbohydrates with metabolic disease. Our study showed that higher carbohydrate intake and lower energy intake were observed in the diabetes group than in the non-diabetes group irrespective of diagnosed or undiagnosed diabetes. Regarding the lower energy intake in the diabetes group, underreporting food intake has been suggested as a problem in diabetic patients [38]. Park [33] investigated the levels of adherence to dietary recommendations between diagnosed and undiagnosed subjects with T2DM in Korea from 1998 to 2012 KNHANES. The overall adherence levels to dietary recommendations were low regardless of awareness of disease. One of the least followed recommendations was moderating carbohydrate consumption. Both diagnosed and undiagnosed T2DM subjects had a low level of adherence in limiting carbohydrate consumption to 50% to 60% of total energy intake, with only 10% to 20% of subjects following this guideline. Carbohydrate intake is higher in the Korean population than in other Asian and Western populations [39,40]. However, another recent report demonstrated that the food sources of energy intake are changing [41]. Nonetheless, carbohydrate intake is still high in Korea. Because there were several limitations to assessing the nutritional patterns of Korean people with diabetes, the data should be interpreted with caution. First, because the study design was crosssectional, we do not know whether the pattern in subjects’ diets would contribute to the development of their disease or has been changed because of their diseases. In addition, the 1-day 24-hour recall report may not reflect the usual dietary intake of the people, and the retrospective assessment of dietary intake may induce some measurement errors. Further longitudinal studies are necessary to understand why diabetic patients showed higher carbohydrate and less energy intake than their nondiabetic counterparts.
- In conclusion, a stable high prevalence of diabetes, a steadily increasing prevalence of IFG, and a low glycemic control rate in people with diabetes were again confirmed. In addition, nearly half of people with diabetes had both hypertension and hypercholesterolemia, and the target achievement rate was still very low. Therefore, more stringent efforts are needed to prevent the development of diabetes and improve the comprehensive management of diabetes to reduce diabetes-related morbidity and mortality.
DISCUSSION
Supplementary Materials
Supplementary Table 1.
Supplementary Fig. 1.
Supplementary Fig. 2.
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: C.H.J., W.J.K., H.S.K., S.J.J., J.O.M.
Acquisition, analysis, or interpretation of data: C.H.J., J.W.S., S.Y.K., H.S.K., M.S., H.J.S., S.S.L., Y.C., S.J.H., H.M.J., M.R., S.L., S.R.K.
Drafting the work or revising: C.H.J., S.J.J., M.K., B.Y., J.W.M., H.Y.L., J.S.Y.
Final approval of the manuscript: C.H.J., W.J.K., H.S.K., S.J.J., S.Y.K., S.R.K., I.K.J., J.O.M., K.H.Y.
-
FUNDING
None
NOTES
-
Acknowledgements
- This study was supported by The Korean Diabetes Association.

| Variable |
Diabetes |
Impaired fasting glucose |
||||
|---|---|---|---|---|---|---|
| Total | Men | Women | Total | Men | Women | |
| By age group, yr | ||||||
| ≥30 | 13.8 (4,940) | 15.9 (2,774) | 11.8 (2,166) | 26.9 (9,485) | 32 (5,535) | 22 (3,951) |
| ≥65 | 27.6 (2,044) | 27.7 (879) | 27.5 (1,165) | 29.6 (2,178) | 31.6 (993) | 28.1 (1,185) |
| 30–39 | 3.7 (95) | 2.7 (143) | 22.9 (410) | 11.4 (891) | ||
| 40–49 | 13.0 (148) | 3.5 (565) | 34 (826) | 19.7 (1,474) | ||
| 50–59 | 17.9 (476) | 11.3 (760) | 39 (1,057) | 25.1 (1,656) | ||
| 60–69 | 25.7 (563) | 19.0 (720) | 31.8 (847) | 28.7 (891) | ||
| ≥70 | 28.8 (883) | 29.4 (586) | 31 (810) | 27.1 (622) | ||
| By family income (quintiles)a | ||||||
| Quintile 1 | 14.4 | 16.8 | 12 | |||
| Quintile 2 | 14 | 17.1 | 10.9 | |||
| Quintile 3 | 10.6 | 11.5 | 9.6 | |||
| Quintile 4 | 10.6 | 13.9 | 7.1 | |||
| Quintile 5 | 8.6 | 11.7 | 5.8 | |||
| Variable | Awareness, % | Treatment, % | Glucose management (<6.5%), % |
|---|---|---|---|
| ≥30 yr | 65 | 60.1 | 28.3 |
| Men | 61.2 | 56.6 | 29.2 |
| Women | 69.8 | 64.6 | 27.2 |
| ≥65 yr | 77.9 | 72.9 | 29.3 |
- 1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019;157:107843.ArticlePubMed
- 2. World Health Organization: Global report on diabetes. Available from: https://apps.who.int/iris/handle/10665/204871 (cited 2020 Dec 18).
- 3. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513-30.PubMedPMC
- 4. World Health Organization: WHO Mortality Database. Available from: https://www.who.int/healthinfo/statistics/mort/en/ (cited 2020 Dec 18).
- 5. Statistics Korea: Causes of death statistics in 2018. Available from: http://kostat.go.kr (cited 2020 Dec 18).
- 6. Organisation for Economic Co-operation and Development (OECD): Health care quality indicators: primary care. Available from: http://www.oecd.org/els/health-systems/hcqi-primarycare.htm (cited 2020 Dec 18).
- 7. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014;43:69-77.ArticlePubMedPMC
- 8. Ministry of Health and Welfare: Korean National Health and Nutrition Examination Survey (KNHANES). Available from: http://knhanes.cdc.go.kr (cited 2020 Dec 18).
- 9. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499-502.ArticlePubMedPDF
- 10. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37 Suppl 1:S81-90.ArticlePubMedPDF
- 11. Oh SW, Shin SA, Yun YH, Yoo T, Huh BY. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res 2004;12:2031-40.ArticlePubMed
- 12. Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J 2019;43:398-406.ArticlePubMedPMCPDF
- 13. Committee of Clinical Practice Guideline of the Korean Society of Lipid and Atherosclerosis. Korean guidelines for the management of dyslipidemia. 4th ed. Seoul: The Korean Society of Lipid and Atherosclerosis; 2018.
- 14. Ministry of Health and Welfare. Dietary reference intakes for Koreans 2015. Sejong: The Korean Nutrition Society; 2015.
- 15. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care 2009;32:2016-20.PubMedPMC
- 16. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J 2011;35:303-8.ArticlePubMedPMC
- 17. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, et al. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J 2013;37:349-57.ArticlePubMedPMC
- 18. Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, et al. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J 2019;43:487-94.ArticlePubMedPMCPDF
- 19. Won JC, Lee JH, Kim JH, Kang ES, Won KC, Kim DJ, et al. Diabetes fact sheet in Korea, 2016: an appraisal of current status. Diabetes Metab J 2018;42:415-24.ArticlePubMedPMCPDF
- 20. Korean Diabetes Association: Diabetes fact sheet in Korea 2020. Available from: https://www.diabetes.or.kr/pro/news/admin.php?category=A&code=admin&number=1972&mode=view (cited 2020 Dec 18).
- 21. Korean Diabetes Association: Diabetes fact sheet in Korea 2012. Available from: https://www.diabetes.or.kr/pro/news/admin.php?category=A&code=admin&number=1972&mode=view (cited 2020 Dec 18).
- 22. Magliano DJ, Islam RM, Barr EL, Gregg EW, Pavkov ME, Harding JL, et al. Trends in incidence of total or type 2 diabetes: systematic review. BMJ 2019;366:l5003.ArticlePubMedPMC
- 23. Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul) 2015;30:142-6.ArticlePubMedPMC
- 24. Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, et al. Prevalence, awareness, and management of obesity in Korea: data from the Korea National Health and Nutrition Examination Survey (1998-2011). Diabetes Metab J 2014;38:35-43.ArticlePubMedPMC
- 25. Chen CM, Yeh MC. The prevalence and determinants of impaired fasting glucose in the population of Taiwan. BMC Public Health 2013;13:1123.ArticlePubMedPMCPDF
- 26. Blum J, Aeschbacher S, Schoen T, Bossard M, Pumpol K, Brasier N, et al. Prevalence of prediabetes according to hemoglobin A1c versus fasting plasma glucose criteria in healthy adults. Acta Diabetol 2015;52:631-2.ArticlePubMedPDF
- 27. Yip WC, Sequeira IR, Plank LD, Poppitt SD. Prevalence of prediabetes across ethnicities: a review of impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) for classification of dysglycaemia. Nutrients 2017;9:1273.ArticlePubMedPMC
- 28. Eades CE, France EF, Evans JM. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur J Public Health 2016;26:699-706.ArticlePubMed
- 29. Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet 2012;379:2279-90.ArticlePubMedPMC
- 30. Kaiser A, Vollenweider P, Waeber G, Marques-Vidal P. Prevalence, awareness and treatment of type 2 diabetes mellitus in Switzerland: the CoLaus study. Diabet Med 2012;29:190-7.ArticlePubMed
- 31. Hu M, Wan Y, Yu L, Yuan J, Ma Y, Hou B, et al. Prevalence, awareness and associated risk factors of diabetes among adults in Xi’an, China. Sci Rep 2017;7:10472.ArticlePubMedPMCPDF
- 32. Cummings KM, Proctor RN. The changing public image of smoking in the United States: 1964-2014. Cancer Epidemiol Biomarkers Prev 2014;23:32-6.ArticlePubMedPMCPDF
- 33. Park K. Trends in adherence to dietary recommendations among Korean type 2 diabetes mellitus patients. Nutr Res Pract 2015;9:658-66.ArticlePubMedPMC
- 34. Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010;375:2215-22.ArticlePubMedPMC
- 35. Ko SH, Kwon HS, Kim DJ, Kim JH, Kim NH, Kim CS, et al. Higher prevalence and awareness, but lower control rate of hypertension in patients with diabetes than general population: the fifth Korean National Health and Nutrition Examination Survey in 2011. Diabetes Metab J 2014;38:51-7.ArticlePubMedPMC
- 36. Korean Diabetes Association. Treatment guideline for diabetes. 6th ed. Seoul: Korean Diabetes Association; 2019.
- 37. Lee YJ, Song S, Song Y. High-carbohydrate diets and food patterns and their associations with metabolic disease in the Korean population. Yonsei Med J 2018;59:834-42.ArticlePubMedPMCPDF
- 38. Salle A, Ryan M, Ritz P. Underreporting of food intake in obese diabetic and nondiabetic patients. Diabetes Care 2006;29:2726-7.ArticlePubMedPDF
- 39. Park SH, Lee KS, Park HY. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). Int J Cardiol 2010;139:234-40.ArticlePubMed
- 40. Lee H, Kim M, Daly BJ. Nutritional patterns of Korean diabetic patients: an exploratory study. Int Nurs Rev 2008;55:442-6.ArticlePubMed
- 41. Yun S, Kim HJ, Oh K. Trends in energy intake among Korean adults, 1998-2015: results from the Korea National Health and Nutrition Examination Survey. Nutr Res Pract 2017;11:147-54.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- 호남권 지역주민의 건강행태와 만성질환 관리현황
선아 김, 정은 이
Public Health Weekly Report.2024; 17(2): 46. CrossRef - Variability in the association of smoking status with the prevalence of diabetes mellitus in the Korean population according to different definitions of smoking status: analysis based on the Korea National Health and Nutrition Examination Survey (2014-202
Yechan Kyung, Young Sook Park, Mi Hyeon Jin, Hae Jeong Lee
International Journal of Environmental Health Research.2024; : 1. CrossRef - Factors Influencing the Dietary Behavior of Patients with Type 2 Diabetes Mellitus: A Cross-sectional Study
Sohyun Jin, Youngshin Song
Journal of Korean Academy of Fundamentals of Nursing.2024; 31(1): 80. CrossRef - Analysis of dietary behavior and intake related to glycemic control in patients with type 2 diabetes aged 30 years or older in Korea: Utilizing the 8th Korea National Health and Nutrition Examination Survey (2019–2021)
Jin-Ah Seok, Yeon-Kyung Lee
Nutrition Research and Practice.2024; 18(2): 239. CrossRef - Exposure to Bisphenol A, S, and F and its Association with Obesity and Diabetes Mellitus in General Adults of Korea: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Min Joo Kim, Inae Lee, Sunmi Kim, Sohyeon Choi, Jeongim Park, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Hyunwoong Park, Gi Jeong Cheon, Young Joo Park, Kyungho Choi
Exposure and Health.2023; 15(1): 53. CrossRef - The evolution and future of diagnostic criteria for diabetes mellitus
Eun-Jung Rhee
Journal of the Korean Medical Association.2023; 66(7): 409. CrossRef - Efficacy of intermittent short‐term use of a real‐time continuous glucose monitoring system in non‐insulin–treated patients with type 2 diabetes: A randomized controlled trial
Sun Joon Moon, Kyung‐Soo Kim, Woo Je Lee, Mi Yeon Lee, Robert Vigersky, Cheol‐Young Park
Diabetes, Obesity and Metabolism.2023; 25(1): 110. CrossRef - Ocular motility disorders following coronavirus disease-19 vaccination
Kyung-Ah Park, Hyeshin Jeon, Dong Gyu Choi, Jae Ho Jung, Hyun-Jin Shin, Byung Joo Lee, Yeji Moon, Se-Youp Lee, Dong Cheol Lee, Soon Young Cho, Seong-Joon Kim, Sei Yeul Oh, Sunghyuk Moon, Shin Yeop Oh, Daye Diana Choi, Mi Young Choi, Won Jae Kim, Ungsoo Sa
Graefe's Archive for Clinical and Experimental Ophthalmology.2023; 261(4): 1127. CrossRef - Comorbidities associated with high-risk obstructive sleep apnea based on the STOP-BANG questionnaire: a nationwide population-based study
Gene Huh, Kyoung do Han, Yong-Moon Park, Chan-Soon Park, Kyu-na Lee, Eun Young Lee, Jung-Hae Cho
The Korean Journal of Internal Medicine.2023; 38(1): 80. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Threshold dose–response association between smoking pack-years and the risk of gallbladder cancer: A nationwide cohort study
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han
European Journal of Cancer.2023; 180: 99. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Momordica charantia (bitter melon) efficacy and safety on glucose metabolism in Korean prediabetes participants: a 12-week, randomized clinical study
Bukyung Kim, Hak Sung Lee, Hye-Jin Kim, Hyolynn Lee, In-young Lee, Soyoung Ock, Sukyoung Kwon, Sang-Soo Kang, Youngsik Choi
Food Science and Biotechnology.2023; 32(5): 697. CrossRef - Dynamic changes in prevalence of type 2 diabetes along with associated factors in Bangladesh: Evidence from two national cross-sectional surveys (BDHS 2011 and BDHS 2017–18)
Sabiha Shirin Sara, Ashis Talukder, Ka Yiu Lee, Nayan Basak, Shaharior Rahman Razu, Iqramul Haq, Chuton Deb Nath
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(2): 102706. CrossRef - Effectiveness of Non-Contact Dietary Coaching in Adults with Diabetes or Prediabetes Using a Continuous Glucose Monitoring Device: A Randomized Controlled Trial
Yeh-Chan Ahn, Yang Seok Kim, Bukyung Kim, Jung Mi Ryu, Myoung Soo Kim, Minkyeong Kang, Jiwon Park
Healthcare.2023; 11(2): 252. CrossRef - Interactions between Bitter Taste Receptor Gene Variants and Dietary Intake Are Associated with the Incidence of Type 2 Diabetes Mellitus in Middle-Aged and Older Korean Adults
Kyung Won Lee, Dayeon Shin
International Journal of Molecular Sciences.2023; 24(3): 2199. CrossRef - Relationship between age at menarche and metabolic diseases in Korean postmenopausal women: The Korea National Health and Nutrition Examination Survey 2016–2018
Hyein Jung, Yeon-Ah Sung, Young Sun Hong, Do Kyeong Song, So-hyeon Hong, Hyejin Lee, Tatsuo Shimosawa
PLOS ONE.2023; 18(1): e0280929. CrossRef - Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
Diabetes & Metabolism Journal.2023; 47(1): 82. CrossRef - Cumulative muscle strength and risk of diabetes: A prospective cohort study with mediation analysis
Shanhu Qiu, Xue Cai, Yan Liang, Wenji Chen, Duolao Wang, Zilin Sun, Bo Xie, Tongzhi Wu
Diabetes Research and Clinical Practice.2023; 197: 110562. CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Consistency of 1-day and 3-day average dietary intake and the relationship of dietary intake with blood glucose, hbA1c, BMI, and lipids in patients with type 2 diabetes
DaeEun Lee, Haejung Lee, Sangeun Lee, MinJin Lee, Ah Reum Khang
Journal of Korean Biological Nursing Science.2023; 25(1): 20. CrossRef - Systematic literature review and meta-analysis of cardiovascular risk factor management in selected Asian countries
Eric J Yeh, Ruth Bartelli Grigolon, Sarah Ramalho Rodrigues, Ana Paula A Bueno
Journal of Comparative Effectiveness Research.2023;[Epub] CrossRef - Gut Microbial Genes and Metabolism for Methionine and Branched-Chain Amino Acids in Diabetic Nephropathy
Ji Eun Kim, Hoonsik Nam, Ji In Park, Hyunjeong Cho, Jangwook Lee, Hyo-Eun Kim, Dong Ki Kim, Kwon Wook Joo, Yon Su Kim, Bong-Soo Kim, Sunghyouk Park, Hajeong Lee, Jan Claesen
Microbiology Spectrum.2023;[Epub] CrossRef - Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study
Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Jeong Mi Seo, Hongjo Choi, Young Ae Kang
BMJ Open.2023; 13(3): e069642. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Impact of abdominal obesity on the risk of glioma development in patients with diabetes: A nationwide population-based cohort study in Korea
Hyunji Sang, Yun Kyung Cho, Kyungdo Han, Eun Hee Koh, Sandar Tin Tin
PLOS ONE.2023; 18(3): e0283023. CrossRef - Associations Between Modifiable Risk Factors and Changes in Glycemic Status Among Individuals With Prediabetes
Salma Nabila, Ji-Eun Kim, Jaesung Choi, JooYong Park, Aesun Shin, Sang-Ah Lee, Jong-koo Lee, Daehee Kang, Ji-Yeob Choi
Diabetes Care.2023; 46(3): 535. CrossRef - Effect of diabetes-specific oral nutritional supplements with allulose on weight and glycemic profiles in overweight or obese type 2 diabetic patients
Jihye Tak, Minkyung Bok, Hyunkyung Rho, Ju Hyun Park, Yunsook Lim, Suk Chon, Hyunjung Lim
Nutrition Research and Practice.2023; 17(2): 241. CrossRef - The effects of hemp seed consumption on depression, anxiety and cognitive improvement based on machine learning
Jung Jea-Bum, Cho Yong-Won , Kim Sang-Yub , Chung Soo-Yeon , Han Kyung-Hoon , Ham Byung-Joo , Han Sung-Hee
Archives of Food and Nutritional Science.2023; 7(1): 032. CrossRef - Development and Adaptability of Smartphone-based Dietary Coaching Program for Patients Undergoing Diabetes and Prediabetes with Continuous Glucose Monitoring Device
Myoung Soo Kim, Jung Mi Ryu, Minkyeong Kang, Jiwon Park, Yeh Chan Ahn, Yang Seok Kim
Journal of Health Informatics and Statistics.2023; 48(1): 36. CrossRef - Risk of Diabetic Complications in Type 2 Diabetes Patients with Dementia: A Population-Based Study Using National Health Insurance Claims Data
Eun Sik Jeong, Ah-Young Kim, Hye-Young Kang
Drug Targets and Therapeutics.2023; 2(1): 49. CrossRef - Type 2 Diabetes Mellitus- and Complication-Related Risk of Nontuberculous Mycobacterial Disease in a South Korean Cohort
Da Som Jeon, Seonok Kim, Mi Ae Kim, Yong Pil Chong, Tae Sun Shim, Chang Hee Jung, Ye-Jee Kim, Kyung-Wook Jo, Paschalis Vergidis, Byung Woo Jhun
Microbiology Spectrum.2023;[Epub] CrossRef - Association of advanced chronic kidney disease with diabetic retinopathy severity in older patients with diabetes: a retrospective cross-sectional study
Geun Woo Lee, Chul Ho Lee, Seong Gyu Kim
Journal of Yeungnam Medical Science.2023; 40(2): 146. CrossRef - RELATIVE RISK OF DIABETES MELLITUS AMONG OBESE POPULATION
Umair Khalid, Khuram Chaudry, Hina Khuram
Pakistan Journal of Rehabilitation.2023; 12(1): 93. CrossRef - Public–Private Partnership: Participants’ Experiences of the Web-Based Registration-and-Management System for Patients with Hypertension and Diabetes Mellitus
Seonah Lee, Nanyoung Song, Suhyun Kim
Healthcare.2023; 11(9): 1297. CrossRef - Anti-Hyperglycemic Effects of Fermented Mealworm Extract on Type 2 Diabetic Mice
Hae-In Lee, Asli Turkyilmaz, Mi-Kyung Lee
Journal of the Korean Society of Food Science and Nutrition.2023; 52(4): 431. CrossRef - A Study on Changes in Nutritional and Blood Conditions Before and After Consumption of Diabetic Soymilk in Elderly Women with Diabetes
Hyo-Jeong Hwang, Soon-Hee Park, Seon-Young Park, Soo-Rin Ahn, Su-Jin Park, Yoo-Jin Lee, Kwang-Jin Chon, Chung-Hwa Song, Dae-Gyun Moon, Kyung-Ok Shin
Journal of the Korean Society of Food Science and Nutrition.2023; 52(4): 341. CrossRef - Developing a Classification Algorithm for Prediabetes Risk Detection From Home Care Nursing Notes
Eunjoo Jeon, Aeri Kim, Jisoo Lee, Hyunsook Heo, Hana Lee, Kyungmi Woo
CIN: Computers, Informatics, Nursing.2023; 41(7): 539. CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Peripheral neuropathy and neuropathic pain in the elderly
Je-Young Shin
Journal of Geriatric Neurology.2023; 2(1): 7. CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - A Novel Salivary Sensor with Integrated Au Electrodes and Conductivity Meters for Screening of Diabetes
Chen-Wei Lin, Yuan-Hsiung Tsai, Yun-Shing Peng, Jen-Tsung Yang, Yen-Pei Lu, Mei-Yen Chen, Chun-Wu Tung
Biosensors.2023; 13(7): 702. CrossRef - Pharmacokinetic Comparison Between a Fixed‐Dose Combination of Empagliflozin L‐Proline/Metformin and Empagliflozin/Metformin in Healthy Korean Subjects
HyunJoon Lee, Jae‐Yong Chung, Kyung‐Sang Yu, Shin‐Jung Park, Soyoung Lee
Clinical Pharmacology in Drug Development.2023; 12(12): 1156. CrossRef - Comparisons of the prediction models for undiagnosed diabetes between machine learning versus traditional statistical methods
Seong Gyu Choi, Minsuk Oh, Dong–Hyuk Park, Byeongchan Lee, Yong-ho Lee, Sun Ha Jee, Justin Y. Jeon
Scientific Reports.2023;[Epub] CrossRef - Comparison of therapeutic efficacy and safety of sitagliptin, dapagliflozin, or lobeglitazone adjunct therapy in patients with type 2 diabetes mellitus inadequately controlled on sulfonylurea and metformin: Third agent study
Jun Hwa Hong, Jun Sung Moon, Kayeon Seong, Soo Lim
Diabetes Research and Clinical Practice.2023; 203: 110872. CrossRef - Predicting micropollutant fate during wastewater treatment using refined classical kinetic model based on quantitative monitoring in multi-metropolitan regions of South Korea
Sung Ho Chae, Seung Ji Lim, Mingizem Gashaw Seid, Wondesen Workneh Ejerssa, Aseom Son, Heejong Son, Sangki Choi, Woongbae Lee, Yunho Lee, Seok Won Hong
Water Research.2023; 245: 120627. CrossRef - Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 538. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Lower HbA1C of glycemic control is associated with higher risk of depressive symptoms in elderly with type 2 diabetes mellitus–A Nationwide Community-based study
Yen-Tze Liu, Wan-Hui Wu, Wei-Ting Tseng, Hsien-Chih Lin, Ming-Shiang Wu, Pei-Fen Chen, I-Chien Wu
Journal of Psychosomatic Research.2023; 174: 111492. CrossRef - Association between HbA1c and hearing loss: a tertiary care center-based study
Hyun Jin Lee, Sung Goo Yoo, Sun Jung Lee, Jae Sang Han, In Young Choi, Kyoung Ho Park
Scientific Reports.2023;[Epub] CrossRef - The Relationship between Alcohol Consumption and Diabetes in Korean Adults
Gi Tae Kim, Jae Woong Sull
Biomedical Science Letters.2023; 29(3): 159. CrossRef - Classification and prediction of the effects of nutritional intake on diabetes mellitus using artificial neural network sensitivity analysis: 7th Korea National Health and Nutrition Examination Survey
Kyungjin Chang, Songmin Yoo, Simyeol Lee
Nutrition Research and Practice.2023; 17(6): 1255. CrossRef - Changes in Soluble Serum CD81 Concentration during an Oral Glucose Tolerance Test in Patients with Diabetes Mellitus and Individuals with Normal Glucose Tolerance
Seon Mee Kang, Jun Choul Lee, Bon Jeong Ku
Diagnostics.2023; 13(23): 3500. CrossRef - Association between diabetes mellitus and cause of death in patients with tuberculosis: A Korean nationwide cohort study
Se Hyun Kwak, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang, Frederick Quinn
PLOS ONE.2023; 18(12): e0295556. CrossRef - The development and effects of a nursing education program for hyperglycemia patient care using standardized patients for nursing students
Jin Lee, Pok Ja Oh
The Journal of Korean Academic Society of Nursing Education.2023; 29(4): 427. CrossRef - Position Statement on the Appropriateness and Significance of Adding the Glycated Hemoglobin Test to the National Health Examination
Ji Hye Kim, Dae Jung Kim, Jaehyun Kim, Sangjoon Park, Kyunghoon Lee, Jun Goo Kang, Eu Jeong Ku, Su Kyoung Kwon, Won Jun Kim, Young Sang Lyu, Jang Won Son, Young Sil Eom, Kyung Ae Lee, Jeongrim Lee, Jung Min Lee, Jung Hwa Lee, Jung Hwa Jung, Hochan Cho, Da
The Journal of Korean Diabetes.2023; 24(4): 178. CrossRef - An association between socioeconomic status and preventive screening for diabetic eye and kidney complications among individuals with type 2 diabetes
Changwoo Shon, Jongnam Hwang
Korean Journal of Health Education and Promotion.2023; 40(5): 27. CrossRef - Increased risk of cancer and cancer-related mortality in middle-aged Korean women with prediabetes and diabetes: a population-based study
Thi Xuan Mai Tran, Soyeoun Kim, Huiyeon Song, Boyoung Park
Epidemiology and Health.2023; 45: e2023080. CrossRef - Relationships between fasting glucose levels, lifestyle factors, and metabolic parameters in Korean adults without diagnosis of diabetes mellitus
Seo Young Kang, Young Sik Kim
Journal of Diabetes.2022; 14(1): 52. CrossRef - Exposure to polycyclic aromatic hydrocarbons and volatile organic compounds is associated with a risk of obesity and diabetes mellitus among Korean adults: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Inae Lee, Hyunwoong Park, Min Joo Kim, Sunmi Kim, Sohyeon Choi, Jeongim Park, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Gi Jeong Cheon, Kyungho Choi, Young Joo Park, Min Kyong Moon
International Journal of Hygiene and Environmental Health.2022; 240: 113886. CrossRef - Trends in intake and sources of dietary protein in Korean adults, 1998–2018
Kyung Won Lee, Dayeon Shin
British Journal of Nutrition.2022; 128(8): 1595. CrossRef - Psychometric Properties of the Korean Version of the Perceived Therapeutic Efficacy Scale for Physical Activity in Adults With Type 2 Diabetes
Moonsun Kim, Chun-Ja Kim, Dae Jung Kim, Elizabeth A. Schlenk
The Science of Diabetes Self-Management and Care.2022; 48(1): 11. CrossRef - Risk factors for hypertension and diabetes comorbidity in a Korean population: A cross-sectional study
Jeong Hee Chi, Bum Ju Lee, Masaki Mogi
PLOS ONE.2022; 17(1): e0262757. CrossRef - Muscle strength and prediabetes progression and regression in middle‐aged and older adults: a prospective cohort study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Duolao Wang, Tongzhi Wu
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 909. CrossRef - Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
Diabetes & Metabolism Journal.2022; 46(1): 81. CrossRef - Effect of Combined Treatment with Catechin and Quercetin on Hepatic Glucose Metabolism in Diabetic Rats
Byoung Rai Lee, Pyoung Sim Park
Journal of the Korean Society of Food Science and Nutrition.2022; 51(1): 12. CrossRef - Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study (Diabetes Metab J 2021;45:675-83)
Tae Jung Oh
Diabetes & Metabolism Journal.2022; 46(1): 160. CrossRef - East Asian perspectives in metabolic and bariatric surgery
Tae Jung Oh, Hyuk‐Joon Lee, Young Min Cho
Journal of Diabetes Investigation.2022; 13(5): 756. CrossRef - Substitution of Carbohydrates for Fats and Risk of Type 2 Diabetes among Korean Middle-Aged Adults: Findings from the Korean Genome and Epidemiology Study
Hye-Ah Lee, Hyesook Park
Nutrients.2022; 14(3): 654. CrossRef - Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study
Hee-Chung Kang, Jae-Seok Hong
Healthcare.2022; 10(2): 334. CrossRef - A deep learning model for screening type 2 diabetes from retinal photographs
Jae-Seung Yun, Jaesik Kim, Sang-Hyuk Jung, Seon-Ah Cha, Seung-Hyun Ko, Yu-Bae Ahn, Hong-Hee Won, Kyung-Ah Sohn, Dokyoon Kim
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(5): 1218. CrossRef - Rheological, textural, and functional characteristics of 3D-printed cheesecake containing guava leaf, green tea, and barley sprout powders
Ye-Eun Park, Jeong Kim, Hyun Woo Kim, Jiyeon Chun
Food Bioscience.2022; 47: 101634. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Osteoporosis or fracture risk associated with thiazolidinedione and proton pump inhibitor co‐administration in patients with type 2 diabetes mellitus
Miyoung Ock, Sera Lee, Hyunah Kim
Journal of Clinical Pharmacy and Therapeutics.2022; 47(7): 1028. CrossRef - Differences in the gut microbiome composition of Korean children and adult samples based on different DNA isolation kits
Changyoon Baek, Woo Jin Kim, JaeWoo Moon, Seo Yoon Moon, Wonsub Kim, Hae-Jin Hu, Junhong Min, Jonghoon Choi
PLOS ONE.2022; 17(3): e0264291. CrossRef - Association between Physical Exercise and Glycated Hemoglobin Levels in Korean Patients Diagnosed with Diabetes
Il Yun, Hye Jin Joo, Yu Shin Park, Eun-Cheol Park
International Journal of Environmental Research and Public Health.2022; 19(6): 3280. CrossRef - Editorial: Management of Diabetes and its Complications: A Focus on Endothelial Dysfunction
Shanhu Qiu, Jianhua Ma, Tongzhi Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - The effect of long working hours on developing type 2 diabetes in adults with prediabetes: The Kangbuk Samsung Cohort Study
Eunhye Seo, Yesung Lee, Eunchan Mun, Dae Hoon Kim, Youshik Jeong, Jaehong Lee, Jinsook Jeong, Woncheol Lee
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - GLP-1 receptor agonists in diabetic kidney disease: current evidence and future directions
Ji Hee Yu, So Young Park, Da Young Lee, Nan Hee Kim, Ji A Seo
Kidney Research and Clinical Practice.2022; 41(2): 136. CrossRef - Prevalence of Type 2 Diabetes Mellitus among Korean Children, Adolescents, and Adults Younger than 30 Years: Changes from 2002 to 2016
Yong Hee Hong, In-Hyuk Chung, Kyungdo Han, Sochung Chung
Diabetes & Metabolism Journal.2022; 46(2): 297. CrossRef - Synergistic association between underweight and type 2 diabetes on the development of laryngeal cancer: a national population-based retrospective cohort study
Oh. Hyeong Lee, Yong-Moon Park, Seung-Hyun Ko, Kyuna Lee, Yeonji Kim, Kyungdo Han, Jung-Hae Cho
BMC Cancer.2022;[Epub] CrossRef - Efficacy of Geumguesingi-hwan (jinkuishenqi-wan, kinkijinki-gan) in decreasing blood glucose levels in patients with uncomplicated type 2 diabetes
Hyun-Jin Choi, Ji-Soo Baek, Cheon-Hoo Jeon, Seon-Mi Shin, Chung-Sik Cho
Medicine.2022; 101(12): e29079. CrossRef - Effect of Motivational Interviewing Training on Diabetes Educators’ Counseling Skills and Self-Efficacy
Sung-Chul Lim
The Journal of Korean Diabetes.2022; 23(1): 57. CrossRef - Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Korean naked waxy barley (saechalssal) extract reduces blood glucose in diabetic mice by modulating the PI3K-Akt-GSK3β pathway
Ju Ri Ham, Young-Jin Son, Yongjin Lee, Hyun-Jin Lee, Jiyoung Yeo, Mi Ja Lee, Mi-Kyung Lee
Biomedicine & Pharmacotherapy.2022; 150: 112976. CrossRef - Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
Ji-Yeon Park, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2022; 37(2): 272. CrossRef - Suicide Risk in Patients With Diabetes Varies by the Duration of Diabetes: The Korea National Health and Nutrition Examination Survey (2019)
Young-Chan Kim, Yoo Hyun Um, Sung-Min Kim, Tae-Won Kim, Ho-Jun Seo, Seung-Chul Hong, Jong-Hyun Jeong
Psychiatry Investigation.2022; 19(4): 326. CrossRef - Gene‐environment interaction in type 2 diabetes in Korean cohorts: Interaction of a type 2 diabetes polygenic risk score with triglyceride and cholesterol on fasting glucose levels
Ji Eun Lim, Ji‐one Kang, Tae‐Woong Ha, Hae‐Un Jung, Dong Jun Kim, Eun Ju Baek, Han Kyul Kim, Ju Yeon Chung, Sang Youl Rhee, Mi Kyung Kim, Yeon‐Jung Kim, Taesung Park, Bermseok Oh
Genetic Epidemiology.2022; 46(5-6): 285. CrossRef - The predictive value of resting heart rate in identifying undiagnosed diabetes in Korean adults: Korea National Health and Nutrition Examination Survey
Dong-Hyuk Park, Wonhee Cho, Yong-Ho Lee, Sun Ha Jee, Justin Y. Jeon
Epidemiology and Health.2022; 44: e2022009. CrossRef - Experiences of Sleep Problems Among Older Korean Immigrants
Yeonsu Song, Gery W. Ryan, Diane Lee, Haesook Kim, Jennifer L. Martin, B. Josea Kramer, Ron D. Hays, Sarah E. Choi
Research in Gerontological Nursing.2022; 15(4): 193. CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Diabetes & Metabolism Journal.2022; 46(3): 355. CrossRef - Exercise, Mitohormesis, and Mitochondrial ORF of the 12S rRNA Type-C (MOTS-c)
Tae Kwan Yoon, Chan Hee Lee, Obin Kwon, Min-Seon Kim
Diabetes & Metabolism Journal.2022; 46(3): 402. CrossRef - Effect of carbohydrate-restricted diets and intermittent fasting on obesity, type 2 diabetes mellitus, and hypertension management: consensus statement of the Korean Society for the Study of obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Clinical Hypertension.2022;[Epub] CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Association of prediabetes with death and diabetic complications in older adults: the pros and cons of active screening for prediabetes
Giwoong Choi, Hojun Yoon, Hyun Ho Choi, Kyoung Hwa Ha, Dae Jung Kim
Age and Ageing.2022;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Correlation of advanced glycation end products and heme oxygenase-1 in Korean diabetic patients
Ha-Neul Choi, Da-Hye Koo, Jung-Eun Yim
Journal of Nutrition and Health.2022; 55(3): 348. CrossRef - The Impact of the Association between Cancer and Diabetes Mellitus on Mortality
Sung-Soo Kim, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(7): 1099. CrossRef - Development and implementation of patient-level prediction models of end-stage renal disease for type 2 diabetes patients using fast healthcare interoperability resources
San Wang, Jieun Han, Se Young Jung, Tae Jung Oh, Sen Yao, Sanghee Lim, Hee Hwang, Ho-Young Lee, Haeun Lee
Scientific Reports.2022;[Epub] CrossRef - Optical-fibre characteristics based on Fano resonances and sensor application in blood glucose detection
Jun Zhu, Jinguo Yin
Optics Express.2022; 30(15): 26749. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 100. CrossRef - Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
Duhoe Kim, Jaehun Seo, Kyoung Hwa Ha, Dae Jung Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 187. CrossRef - Prevalence of Diabetic Retinopathy in Undiagnosed Diabetic Patients: A Nationwide Population-Based Study
Han Na Jang, Min Kyong Moon, Bo Kyung Koo
Diabetes & Metabolism Journal.2022; 46(4): 620. CrossRef - Reproductive Life Span and Severe Hypoglycemia Risk in Postmenopausal Women with Type 2 Diabetes Mellitus
Soyeon Kang, Yong-Moon Park, Dong Jin Kwon, Youn-Jee Chung, Jeong Namkung, Kyungdo Han, Seung-Hyun Ko
Diabetes & Metabolism Journal.2022; 46(4): 578. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - The Association of Pachydrusen Characteristics with Choroidal Thickness and Patient’s Age in Polypoidal Choroidal Vasculopathy versus Central Serous Chorioretinopathy
Young Ho Kim, Yoo-Ri Chung, Chungwoon Kim, Kihwang Lee, Won Ki Lee
International Journal of Molecular Sciences.2022; 23(15): 8353. CrossRef - Experiences of Using Wearable Continuous Glucose Monitors in Adults With Diabetes: A Qualitative Descriptive Study
Hee Sun Kang, Hyang Rang Park, Chun-Ja Kim, Savitri Singh-Carlson
The Science of Diabetes Self-Management and Care.2022; 48(5): 362. CrossRef - Prediction Model for Hypertension and Diabetes Mellitus Using Korean Public Health Examination Data (2002–2017)
Yong Whi Jeong, Yeojin Jung, Hoyeon Jeong, Ji Hye Huh, Ki-Chul Sung, Jeong-Hun Shin, Hyeon Chang Kim, Jang Young Kim, Dae Ryong Kang
Diagnostics.2022; 12(8): 1967. CrossRef - Recent Increases in Influenza-Related Hospitalizations, Critical Care Resource Use, and In-Hospital Mortality: A 10-Year Population-Based Study in South Korea
Tae Hwa Hong, Hyung Seok Lee, Nam-Eun Kim, Kyu Jin Lee, Yong Kyun Kim, Jung Nam An, Joo-Hee Kim, Hyung Won Kim, Sunghoon Park
Journal of Clinical Medicine.2022; 11(16): 4911. CrossRef - Clinical and economic impact of changing reimbursement criteria for statin treatment among patients with type 2 diabetes mellitus in South Korea
Siin Kim, Kyungseon Choi, Ji-yool Kim, Hae Sun Suh
Frontiers in Pharmacology.2022;[Epub] CrossRef - Experience of Elderly Korean Women with Diabetes and Multimorbidity in Elderly Couple Households: A Qualitative Study
Oksoo Kim, Hyunju Dan
Healthcare.2022; 10(9): 1675. CrossRef - Long-Term Changes in HbA1c According to Blood Glucose Control Status During the First 3 Months After Visiting a Tertiary University Hospital
Hyunah Kim, Da Young Jung, Seung-Hwan Lee, Jae-Hyoung Cho, Hyeon Woo Yim, Hun-Sung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Sex and Diet-Related Disparities in Low Handgrip Strength among Young and Middle-Aged Koreans: Findings Based on the Korea National Health and Nutrition Examination Survey (KNHANES) from 2014 to 2017
Inhye Kim, Kumhee Son, Su Jin Jeong, Hyunjung Lim
Nutrients.2022; 14(18): 3816. CrossRef - Rising Incidence of Diabetes in Young Adults in South Korea: A National Cohort Study
Hyun Ho Choi, Giwoong Choi, Hojun Yoon, Kyoung Hwa Ha, Dae Jung Kim
Diabetes & Metabolism Journal.2022; 46(5): 803. CrossRef - Analysis of the Association between Metabolic Syndrome and Renal Function in Middle-Aged Patients with Diabetes
Yoonjin Park, Su Jung Lee
International Journal of Environmental Research and Public Health.2022; 19(18): 11832. CrossRef - Exploring the risk factors of impaired fasting glucose in middle-aged population living in South Korean communities by using categorical boosting machine
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Body mass index and stroke risk among patients with diabetes mellitus in Korea
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Tariq Jamal Siddiqi
PLOS ONE.2022; 17(9): e0275393. CrossRef - Low relative hand grip strength is associated with a higher risk for diabetes and impaired fasting glucose among the Korean population
Min Jin Lee, Ah Reum Khang, Dongwon Yi, Yang Ho Kang, Giacomo Pucci
PLOS ONE.2022; 17(10): e0275746. CrossRef - Association of Glycosylated Hemoglobin Level and Cancer-Related Mortality in Patients without Diabetes
Tae Kyung Yoo, Mi Yeon Lee, Sul A. Lee, Eun Sun Cheong, Mi Hae Seo, Ki Chul Sung
Journal of Clinical Medicine.2022; 11(19): 5933. CrossRef - Risk of Carotid Atherosclerosis in Subjects with Prediabetes Overlapping Metabolic Syndrome
Seol A Jang, Kyoung Min Kim, Seok Won Park, Chul Sik Kim
Metabolic Syndrome and Related Disorders.2022; 20(10): 599. CrossRef - Lifestyle changes and risk of tuberculosis in patients with type 2 diabetes mellitus: A nationwide cohort study
Jiho Park, Ji Hyun Yoon, Hyun Kyun Ki, Kyungdo Han, Hyungjin Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
Journal of the Korean Fracture Society.2022; 35(4): 135. CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Musculoskeletal complications in patients with diabetes mellitus
Jong Han Choi, Hae-Rim Kim, Kee-Ho Song
The Korean Journal of Internal Medicine.2022; 37(6): 1099. CrossRef - Blood Biochemical Characteristics, Dietary Intake, and Risk Factors Related to Poor HbA1c Control in Elderly Korean Diabetes Patients: Comparison between the 4th(2007-2009) and the 7th(2016-2018) Korea National Health and Nutrition Examination Surveys
Sung-Won Oh, Sook-Bae Kim
Korean Journal of Community Nutrition.2022; 27(5): 406. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - Brachial-ankle pulse wave velocity as a predictor of long-term cardiovascular events in 2174 subjects with type 2 diabetes mellitus: A retrospective cohort study
Hack-Lyoung Kim, Won Kyeong Jeon, Hyun Sung Joh, Woo-Hyun Lim, Jae-Bin Seo, Sang-Hyun Kim, Joo-Hee Zo, Myung-A Kim
Medicine.2022; 101(45): e31758. CrossRef - Artificial Intelligence-based Prediction of Diabetes and Prediabetes Using Health Checkup Data in Korea
Hyeonseop Yuk, Juhui Gim, Jung Kee Min, Jaesuk Yun, Tae-Young Heo
Applied Artificial Intelligence.2022;[Epub] CrossRef - Sex Differences in the Effects of CDKAL1 Variants on Glycemic Control in Diabetic Patients: Findings from the Korean Genome and Epidemiology Study
Hye Ah Lee, Hyesook Park, Young Sun Hong
Diabetes & Metabolism Journal.2022; 46(6): 879. CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Classification of Type 2 Diabetes Incidence Risk and the Health Behavior of the 30–50-Year-Old Korean Adults: Latent Class Analysis
Roma Seol, Jin-Ho Chun
International Journal of Environmental Research and Public Health.2022; 19(24): 16600. CrossRef - Association between Amount of Alcohol Consumption and Serum Fasting Glucose Level in Korean Male in their 40s and 50s: The Seventh Korea National Health and Nutrition Examination Survey 2016-2018
Jihyun Kim
Korean Journal of Family Practice.2022; 12(5): 320. CrossRef - Associated Factors with Health-related Quality of Life among Older Adults with Diabetes in Korea
Eun-Kyung Lee, Sun-Young Jung
The Korean Journal of Rehabilitation Nursing.2022; 25(2): 61. CrossRef - Chronic Disease Prediction Using the Common Data Model: Development Study
Chanjung Lee, Brian Jo, Hyunki Woo, Yoori Im, Rae Woong Park, ChulHyoung Park
JMIR AI.2022; 1(1): e41030. CrossRef - Threshold Dose-Response Association between Smoking Pack-Years and the Risk of Gallbladder Cancer: A Nationwide Cohort Study
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han
SSRN Electronic Journal .2022;[Epub] CrossRef - The risk of stroke according to statin medication compliance in older people with chronic periodontitis: an analysis using the Korea National Health Insurance Service-Senior Cohort Database
Seon-Rye Kim, Minkook Son, Yu-Rin Kim
Epidemiology and Health.2022; 44: e2022055. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef - Treatment Patterns of Type 2 Diabetes Assessed Using a Common Data Model Based on Electronic Health Records of 2000–2019
Kyung Ae Lee, Heung Yong Jin, Yu Ji Kim, Yong-Jin Im, Eun-Young Kim, Tae Sun Park
Journal of Korean Medical Science.2021;[Epub] CrossRef - Factors Associated with Depressive Symptoms in Korean Adults with Diabetes Mellitus: A Cross-Sectional Study
Mihyun Jeong
Healthcare.2021; 9(8): 1049. CrossRef - Young-onset type 2 diabetes in South Korea: a review of the current status and unmet need
Ye Seul Yang, Kyungdo Han, Tae Seo Sohn, Nam Hoon Kim
The Korean Journal of Internal Medicine.2021; 36(5): 1049. CrossRef - Metabolic Effects of Gastrectomy and Duodenal Bypass in Early Gastric Cancer Patients with T2DM: A Prospective Single-Center Cohort Study
Young Ki Lee, Eun Kyung Lee, You Jin Lee, Bang Wool Eom, Hong Man Yoon, Young-Il Kim, Soo Jeong Cho, Jong Yeul Lee, Chan Gyoo Kim, Sun-Young Kong, Min Kyong Yoo, Yul Hwangbo, Young-Woo Kim, Il Ju Choi, Hak Jin Kim, Mi Hyang Kwak, Keun Won Ryu
Journal of Clinical Medicine.2021; 10(17): 4008. CrossRef - Sex- and Age-Specific Trends in Cardiovascular Health in Korea, 2007–2018
So Mi Jemma Cho, Hokyou Lee, Hyeon Chang Kim
Korean Circulation Journal.2021; 51(11): 922. CrossRef - Efficacy and Safety of Switching to Teneligliptin in Patients with Type 2 Diabetes Inadequately Controlled with Dipeptidyl Peptidase-4 Inhibitors: 52-Week Results from a Prospective Observational Study
Hae Jin Kim, Young Sik Kim, Chang Beom Lee, Moon-Gi Choi, Hyuk-Jae Chang, Soo Kyoung Kim, Jae Myung Yu, Tae Ho Kim, Ji Hyun Lee, Kyu Jeung Ahn, Kyung Wan Min, Eun Jung Kyung, Yeo Kyeong Kim, Kwan Woo Lee
Diabetes Therapy.2021; 12(11): 2907. CrossRef - RANTES 59029A/G Polymorphisms Associated with Diabetic Compilations in Korean Patients with Type 2 Diabetes for over 15 Years
Dong-Hwa Lee, Eu-Jeong Ku, Tae-Keun Oh, Hyun-Jeong Jeon
Genes.2021; 12(9): 1445. CrossRef - Combination of Statin and Ezetimibe versus Statin Monotherapy on Cardiovascular Disease and Type 2 Diabetes Incidence among Adults with Impaired Fasting Glucose: a Propensity-Matched Nationwide Cohort Study
You-Bin Lee, Bongsung Kim, Kyungdo Han, Jung A Kim, Eun Roh, So-hyeon Hong, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Journal of Lipid and Atherosclerosis.2021; 10(3): 303. CrossRef - A Century of Progress in Diabetes Care with Insulin: A History of Innovations and Foundation for the Future
Seung-Hwan Lee, Kun-Ho Yoon
Diabetes & Metabolism Journal.2021; 45(5): 629. CrossRef - Proteinuria as a significant predictive factor for the progression of carotid artery atherosclerosis in non-albuminuric type 2 diabetes
Young-eun Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes Research and Clinical Practice.2021; 181: 109082. CrossRef - Symptom Clusters and Quality of Life in Patients with Type 2 Diabetes Mellitus
Su-Yeon Hong, Yang-Sook Yoo
Korean Journal of Adult Nursing.2021; 33(5): 498. CrossRef - The association between triglyceride-glucose index, cardio-cerebrovascular diseases, and death in Korean adults: A retrospective study based on the NHIS-HEALS cohort
Joungyoun Kim, Sang-Jun Shin, Hee-Taik Kang, Claudio Passino
PLOS ONE.2021; 16(11): e0259212. CrossRef - Effect of Breastfeeding and Its Duration on Impaired Fasting Glucose and Diabetes in Perimenopausal and Postmenopausal Women: Korea National Health and Nutrition Examination Survey (KNHANES) 2010–2019
Byung-Soo Kwan, In-Ae Cho, Ji-Eun Park
Medicines.2021; 8(11): 71. CrossRef - The Correlation between Carotid Intima-Media Thickness and Neutrophil to Lymphocyte Ratio in Prediabetes Patients
Dayoung Lee, Mi-Jeong Park, Mee Young Kim, Jung Jin Cho, Jong Lull Yoon
Korean Journal of Family Medicine.2021; 42(6): 464. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Restoration for the foregut surgery: bridging gaps between foregut surgery practice and academia
Ye-lim Shin, Shin-Hoo Park, Yeongkeun Kwon, Chang Min Lee, Sungsoo Park
Journal of Minimally Invasive Surgery.2021; 24(4): 175. CrossRef - Prevalence and Treatment of Diabetes in China, 2013-2018
Limin Wang, Wen Peng, Zhenping Zhao, Mei Zhang, Zumin Shi, Ziwei Song, Xiao Zhang, Chun Li, Zhengjing Huang, Xiaomin Sun, Linhong Wang, Maigeng Zhou, Jing Wu, Youfa Wang
JAMA.2021; 326(24): 2498. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
Seung-Hyun Ko
The Journal of Korean Diabetes.2021; 22(4): 244. CrossRef - Spatiotemporal analyses of the epidemiological characteristics of diabetes mellitus
Sang Youl Rhee
Epidemiology and Health.2021; 43: e2021102. CrossRef - Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
Harim Choe, Hoyong Sung, Geon Hui Kim, On Lee, Hyo Youl Moon, Yeon Soo Kim
Epidemiology and Health.2021; 43: e2021080. CrossRef

 KDA
KDA PubReader
PubReader ePub Link
ePub Link Cite
Cite