
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 37(1); 2013 > Article
-
Original ArticleObesity and Metabolic Syndrome Increased Selenoprotein P Levels in Subjects with Visceral Obesity and Nonalcoholic Fatty Liver Disease
- Hae Yoon Choi1, Soon Young Hwang2, Chang Hee Lee3, Ho Cheol Hong1, Sae Jeong Yang1, Hye Jin Yoo1, Ji A Seo1, Sin Gon Kim1, Nan Hee Kim1, Sei Hyun Baik1, Dong Seop Choi1, Kyung Mook Choi1
-
Diabetes & Metabolism Journal 2013;37(1):63-71.
DOI: https://doi.org/10.4093/dmj.2013.37.1.63
Published online: February 15, 2013
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
2Department of Biostatistics, Korea University College of Medicine, Seoul, Korea.
3Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- Corresponding author: Kyung Mook Choi. Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, 148 Gurodong-ro, Guro-gu, Seoul 152-703, Korea. medica7@gmail.com
Copyright © 2013 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Selenoprotein P (SeP) has recently been reported as a novel hepatokine that regulates insulin resistance and systemic energy metabolism in rodents and humans. We explored the associations among SeP, visceral obesity, and nonalcoholic fatty liver disease (NAFLD).
-
Methods
- We examined serum SeP concentrations in subjects with increased visceral fat area (VFA) or liver fat accumulation measured with computed tomography. Our study subjects included 120 nondiabetic individuals selected from participants of the Korean Sarcopenic Obesity Study. In addition, we evaluated the relationship between SeP and cardiometabolic risk factors, including homeostasis model of insulin resistance (HOMA-IR), high sensitivity C-reactive protein (hsCRP), adiponectin values, and brachial-ankle pulse wave velocity (baPWV).
-
Results
- Subjects with NAFLD showed increased levels of HOMA-IR, hsCRP, VFA, and several components of metabolic syndrome and decreased levels of adiponectin and high density lipoprotein cholesterol than those of controls. Serum SeP levels were positively correlated with VFA, hsCRP, and baPWV and negatively correlated with the liver attenuation index. Not only subjects with visceral obesity but also those with NAFLD exhibited significantly increased SeP levels (P<0.001). In multiple logistic regression analysis, the subjects in the highest SeP tertile showed a higher risk for NAFLD than those in the lowest SeP tertile, even after adjusting for potential confounding factors (odds ratio, 7.48; 95% confidence interval, 1.72 to 32.60; P=0.007).
-
Conclusion
- Circulating SeP levels were increased in subjects with NAFLD as well as in those with visceral obesity and may be a novel biomarker for NAFLD.
- Nonalcoholic fatty liver disease (NAFLD), a disease spectrum that includes simple steatosis, nonalcoholic steatohepatitis (NASH) and cirrhosis, has been increasingly recognized as the hepatic manifestation of metabolic syndrome [1]. Visceral obesity is an essential component of metabolic syndrome and a risk factor for type 2 diabetes and cardiovascular diseases [2]. Furthermore, increased visceral fat induces systemic low-grade inflammation, contributing to the development of insulin resistance in humans and mice [3]. Both inflammation and insulin resistance are considered to be pivotal pathogenic mechanisms of NAFLD, as well as metabolic syndrome, type 2 diabetes, and atherosclerosis [4].
- There is mounting evidence implicating adipokines secreted from adipose tissue in the pathogenesis and progression of NAFLD, in addition to the development of insulin resistance and inflammation [5]. In previous studies, including one by the current authors, decreased circulating adiponectin levels have been found in subjects with NAFLD and appear to be inversely related to hepatic insulin resistance, hepatic fat content, and degree of liver inflammation [6,7]. Furthermore, we recently found that retinol binding protein 4, a novel adipokine associated with insulin resistance, appears to be significantly associated with NAFLD [8]. Analogous to adipose tissue, it is hypothesized that the liver may regulate systemic energy metabolism through production of secretory proteins known as hepatokines. In fact, several previous studies have demonstrated that hepatokines, such as fetuin-A and fibroblast growth factor 21 (FGF21), are associated with NAFLD. Stefan et al. [9] showed that high fetuin-A levels are associated with insulin resistance in humans and are elevated in subjects with fat accumulation in the liver. Moreover, Dushay et al. [10] reported that FGF21 values correlate with body mass index (BMI) and may be a novel biomarker for NAFLD.
- Selenoprotein P (SeP) is a secretory protein primarily produced and released by the liver [11]. Recently, Misu et al. [12] found that hepatic SeP mRNA expression was increased in subjects with type 2 diabetes. Furthermore, administration of SeP aggravated insulin resistance in both hepatocytes and myocytes. Conversely, both genetic deletion and RNA interference-mediated knockdown of SeP improved insulin sensitivity and glucose tolerance in mice. Therefore, they concluded that SeP may be a promising target for the treatment of insulin resistance-associated diseases [12]. In our recent study, we also found that circulating SeP concentrations were elevated according to glucose metabolism dysregulation and were related to various cardiometabolic parameters including insulin resistance, inflammation, and atherosclerosis [13]. On the other hand, Zhang and Chen [14] recently demonstrated that SeP has a major role in adipocyte differentiation through the regulation of oxidative stress and inflammatory response. Although previous studies have shown a close relationship among insulin resistance, inflammation, and NAFLD, as far as we know, there is no previous report evaluating the association between SeP and NAFLD.
- In the present study, we examined serum SeP levels in subjects with increased visceral fat area (VFA) or liver fat accumulation measured with computed tomography (CT). Our study participants were nondiabetic Korean subjects selected from an ongoing prospective observational cohort study. Furthermore, we evaluated the relationship between SeP levels and cardiometabolic risk factors, including homeostasis model of insulin resistance (HOMA-IR) values, high sensitivity C-reactive protein (hsCRP) levels, adiponectin concentrations, and arterial stiffness measured with brachial-ankle pulse wave velocity (baPWV).
INTRODUCTION
- Subjects and data collection
- Study subjects were selected from the participants of the Korean Sarcopenic Obesity Study (KSOS), an ongoing epidemiologic study supported by the Korea Science and Engineering Foundation (KOSEF). This prospective observational cohort study was designed to examine the prevalence of sarcopenia and sarcopenic obesity in Korean adults with or without diabetes and to evaluate their effects on metabolic disorders and health outcomes; details have been previously published [15,16]. Participants were enrolled in the KSOS cohort between September 2007 and August 2009, and a follow-up survey was conducted thereafter. Study participants included 446 well-functioning, community-dwelling, healthy volunteers without diabetes recruited from residents of Seoul, Korea and 428 diabetic patients being treated at the Diabetes Center of Korea University Guro Hospital. No participants had a history of cardiovascular disease (myocardial infarction, unstable angina, stroke, or cardiovascular revascularization), stage 2 hypertension (resting blood pressure, ≥160/100 mm Hg), malignancy, or severe renal or hepatic disease. Subjects taking medications that might affect body weight or body composition were excluded. For this study, we excluded diabetic subjects to eliminate possible confounding effects because a previous study reported increased SeP concentrations in diabetic subjects [12]. In addition, the following exclusion criteria were also used: alcohol consumption >20 g/day in men and >10 g/day in women, a positive test for hepatitis B surface antigen or hepatitis C antibody, and use of herbal medications within the previous 6 months. Among the nondiabetic subjects, 76 subjects had NAFLD by applying our definition. Finally, 60 subjects with NAFLD and 60 age- and sex-matched controls were selected from the nondiabetic KSOS participants using the baseline data for abdominal CT and other epidemiological characteristics. All participants provided written informed consent, and the Korea University Institutional Review Board, in accordance with the Declaration of Helsinki of the World Medical Association, approved the study protocol.
- Anthropometric and laboratory measurements
- We calculated BMI as weight/height2 (kg/m2), and waist circumference was measured at the midpoint between the lower border of the rib cage and iliac crest. All blood samples were obtained in the morning following an 8-hour overnight fast and were immediately stored at -70℃ for subsequent assays. Serum triglyceride and high density lipoprotein cholesterol (HDL-C) levels were determined enzymatically using a chemistry analyzer (Hitachi 747; Hitachi, Tokyo, Japan). Low density lipoprotein cholesterol (LDL-C) concentrations were estimated using the Friedewald formula, and a glucose oxidase method was employed to measure plasma glucose levels. Levels of hsCRP and serum insulin were measured with two different electrochemiluminescence immunoassays (Daiichi Pure Chemicals Co., Tokyo, Japan; Roche Diagnostics, Basel, Switzerland). The homeostasis model assessment estimate of insulin resistance (HOMA-IR) was calculated from plasma insulin and glucose values. Serum adiponectin levels were measured with an enzyme linked immunosorbent assay (ELISA, Mesdia, Seoul, Korea), and the intra-assay and inter-assay coefficients of variation (CV) were 5.0% in both cases. Serum SeP levels were determined using a commercially available human ELISA kit (USCN Life Science, Wuhan, China) with an intra-assay CV of 6.7% and an inter-assay CV of 4.7%.
- CT
- Abdominal VFA and total abdominal fat area were measured via CT scan without an intravenous contrast agent (Brilliance 64; Philips Medical Systems, Cleveland, OH, USA). With the subject in the supine position, a 3-mm CT slice scan was acquired at the L4 to L5 level to measure visceral fat and total abdominal fat areas. The cross-sectional surface areas (in cm2) of different abdominal fat compartments were calculated from this slice using commercially available CT software (Rapidia 2.8; INFINITT, Seoul, Korea). We were able to determine adipose tissue area electronically by setting the attenuation values for a region of interest within the range of -190 to -30 Hounsfield units (HU). The VFA was quantified by measuring the intra-abdominal cavity at the internal aspect of the abdominal and oblique muscle walls surrounding the cavity and the posterior aspect of the vertebral body. Subcutaneous fat area (SCFA) was calculated by subtracting VFA from total fat area. Visceral obesity was defined as a VFA of more than 100 cm2 [17].
- Definition of NAFLD
- NAFLD was diagnosed using an unenhanced CT, read by one experienced radiologist who was blinded to the anthropometric and laboratory data. Hepatic attenuation was measured by means of a random selection of three circular regions of interest (ROI) on five transverse sections. To provide an internal control, mean splenic attenuation was also calculated by averaging two random ROI values for the splenic attenuation measurement on transverse section levels. The liver attenuation index (LAI), derived from the difference between the mean hepatic and splenic attenuation, was used as a parameter for the diagnosis of NAFLD. Histologic confirmation of NAFLD requires a minimum of 5% steatosis [18]. Limanond et al. [19] documented that the degree of steatosis correlated very well with the LAI (r=0.92), and that an LAI <5 HU correctly predicted >5% steatosis. Therefore, NAFLD in the present study was defined a value of LAI <5 HU. We recently reported the cutoff points of abdominal obesity indices in screening for NAFLD defined using this criterion [20].
- Pulse wave velocity
- The following variables were measured with a Colin waveform analyzer (model BP-203RPE II; Colin, Komaki, Japan). Extremity blood pressure was measured with the oscillometric method, and ankle-brachial pressure index (ABI) was automatically calculated. Right brachial-ankle pulse wave velocity (rt. baPWV: right upper arm-right ankle), left brachial-ankle pulse wave velocity (lt. baPWV: right upper arm-left ankle), and mean baPWV were also measured and calculated. The reproducibility of this method was reported in our previous study [21].
- Statistical analysis
- Data are expressed as mean±standard deviation, median (interquartile range), or as percentages. Differences between groups were tested using an independent two-sample t-test or the Mann-Whitney U test for continuous variables, and the Pearson chi-squared test was used to test for differences in the distribution of categorical variables. Differences between tertile groups were tested using the one-way analysis of variance (ANOVA) test, Kruskal-Wallis' H-test for continuous variables, and Fisher's exact test or Pearson's chi-squared test for categorical variables. Spearman rank correlation tests were performed to determine the relationships between serum SeP levels and other variables. Odds ratios (OR) (95% confidence interval [CI]) predicting NAFLD based on SeP tertiles, were obtained from logistic regression models after controlling for potential covariates, such as age, sex, BMI, smoking status, blood pressure, triglyceride, HDL-C, adiponectin, hsCRP, and HOMA-IR levels. Data were analyzed using SPSS for Windows version 12.0 (SPSS Inc., Chicago, IL, USA) and SAS for Windows version 9.0 (SAS Institute Inc., Cary, NC, USA). A P value of less than 0.05 indicated statistical significance.
METHODS
- Clinical and laboratory characteristics of the participants
- The clinical and metabolic characteristics of the participants are summarized in Table 1. Although age and sex distributions did not differ between groups, subjects with NAFLD had significantly higher BMI, waist circumference, systolic blood pressure, total cholesterol, triglycerides, aspartate aminotransferase, alanine aminotransferase, HOMA-IR, hsCRP, VFA, and SCFA values and lower HDL-C and adiponectin levels than those of the control group.
- Clinical and laboratory parameters according to SeP tertile
- Table 2 presents the clinical and laboratory variables stratified by SeP level tertile. BMI, waist circumference, systolic blood pressure, triglycerides, HOMA-IR, hsCRP, baPWV, VFA, and SCFA levels increased significantly with increasing SeP levels. Interestingly, subjects with NAFLD (P<0.001), as well as those with visceral obesity (P<0.001) exhibited increased SeP concentrations compared to the control group (Fig. 1).
- Correlation between SeP level and cardiometabolic risk factors
- Circulating SeP levels showed a significant positive correlation with VFA measured with abdominal CT (r=0.338, P<0.001) and a negative correlation with LAI (r=-0.333, P<0.001), which inversely reflects hepatic fat accumulation. Furthermore, SeP concentrations revealed a significant positive correlation with both hsCRP levels (r=0.749, P<0.001) and baPWV (r=0.262, P=0.004).
- Multiple logistic regression analysis of the association between SeP and NAFLD
- Multiple logistic regression analysis was performed using NAFLD as a dependent variable and SeP as an independent variable (Table 3). In the unadjusted model, subjects in the highest SeP tertile showed a higher risk of NAFLD compared to those in the lowest SeP tertile (OR, 10.55; 95% CI, 3.73 to 29.84; P<0.001). Furthermore, multivariate analysis revealed that the association between NAFLD and SeP levels remained significant even after adjusting for potential confounders such as age, sex, BMI, current smoking status, blood pressure, triglycerides, HDL-C, hsCRP, adiponectin, and HOMA-IR values (OR, 7.48; 95% CI, 1.72 to 32.60, highest vs. lowest SeP tertile; P=0.007).
RESULTS
- The present study demonstrates that circulating SeP concentrations appear to be significantly increased in subjects with visceral obesity. In addition, SeP levels appear to be significantly correlated with cardiometabolic risk factors, such as waist circumference, VFA, HOMA-IR, hsCRP, and baPWV values of arterial stiffness. Furthermore, subjects in the highest SeP tertile showed a 7.5 times greater risk of NAFLD than those in the lowest SeP tertile, even after adjustments for age, sex, BMI, and other confounding factors.
- NAFLD is now the leading cause of liver disease in developed countries, with an estimated prevalence of 20% to 35% in the general population [22]. NAFLD is a strong predictor of NASH and also predicts liver cirrhosis, end-stage liver disease, and hepatocellular carcinoma [23]. The development of NAFLD is closely related to visceral obesity, insulin resistance, and other components of metabolic syndrome [22]. Pathogenesis of NAFLD was traditionally explained using the "two-hit theory," [24] whereby the primary insult was accompanied by fat accumulation in hepatocytes and increased oxidative stress. These occurrences lead to inflammation, which induces the second "hit" in the progression to NASH or liver cirrhosis [24].
- Recent studies have revealed the role of hepatokines, novel factors secreted from the liver under excess fat accumulation, that are involved in the regulation of systemic energy metabolism [23]. Fat accumulation in the liver induces the production of the glycoprotein fetuin-A, which aggravates insulin resistance, represses adiponectin production, and induces subclinical inflammation [9,25]. Furthermore, Stefan et al. [9] reported that plasma fetuin-A levels are elevated in subjects with fat accumulation in the liver. Reinehr and Roth [26] also observed that fetuin-A levels were higher in children with NAFLD and were related to insulin resistance and to features of metabolic syndrome. On the other hand, FGF21 is a hepatic protein that plays a critical role in systemic metabolism, and circulating FGF21 levels are increased in subjects with obesity, diabetes, or metabolic syndrome [27]. Yilmaz et al. [28] reported that serum FGF21 levels are increased in subjects with NAFLD regardless of potential confounders.
- Misu et al. [12] recently reported that hepatic SeP mRNA expression was significantly upregulated in subjects with type 2 diabetes according to serial analysis of gene expression and DNA chip methods. Treatment with SeP impaired insulin signaling in hepatocytes and myocytes both in vitro and in vivo. Moreover, knockdown of SeP in the liver or SeP-deficient mice led to improved glucose tolerance and insulin resistance. As a mechanism, they found that the metabolic actions of SeP were mediated by inactivation of adenosine monophosphate-activated protein kinase. Therefore, they concluded that the liver-derived secretory protein SeP may be a target for the treatment of insulin-resistance-associated diseases, including type 2 diabetes [12]. In this study, we found for the first time that novel hepatokine SeP concentrations were significantly correlated with LAI and were increased in subjects with NAFDL regardless of potential confounding factors. LAI is an objective parameter that has a very close quantitative correlation with histologic steatosis [19]. In our previous study, LAI showed a correlation with various anthropometric and metabolic parameters associated with metabolic syndrome [20].
- Recent studies using proton magnetic resonance spectroscopy have shown that hepatic lipid content is directly correlated with visceral fat [29]. In this study, SeP concentration was significantly associated with VFA, and subjects with visceral obesity showed increased circulating SeP levels compared to controls. The strong correlation of VFA with liver fat may be attributable to dysregulated adipokine production via a reduced production of adiponectin and increased productions of tumor necrosis factor-α and interleukin-6 [23]. In the present study, adiponectin concentrations were significantly decreased in subjects with NAFLD compared to the levels in the controls, a finding that is compatible with previous studies. However, the correlation between circulating adiponectin and SeP levels was not significant in our study subjects (r=-0.226, P=0.085). Further studies may be needed to elucidate the relationship and interactions between SeP and adiponectin.
- Recently, NAFLD has emerged as an independent risk factor for cardiovascular disease. Several studies have reported increased carotid intima-media thickness and carotid plaque in subjects with NAFLD [30]. The present study demonstrated that circulating SeP levels appear to be significantly associated with arterial stiffness, as well as hepatic fat accumulation, in subjects without cardiovascular disease. Arterial stiffness measured with baPWV is a useful marker for the assessment of increased cardiovascular disease risk. Many previous studies have reported that arterial stiffness appears to be an independent risk factor for cardiovascular disease and subsequent mortality [31]. Previously, we observed that baPWV is closely associated with inflammatory markers as well as cardiometabolic risk factors of metabolic syndrome [32,33]. Moreover, the present study showed a close correlation between SeP and hsCRP levels (r=0.749, P<0.001), which has emerged as the most powerful inflammatory marker of future cardiovascular risk [34]. Considering the close relationship between SeP and cardiovascular risk factors, such as inflammation, type 2 diabetes and visceral obesity, these results may support the role of SeP in the linkage between NAFLD and atherosclerosis.
- Our study has several limitations to be considered. First, it was performed using baseline data from an ongoing prospective cohort study; therefore, it is not possible to define causality. We are planning to perform a follow-up survey to explore the longitudinal effects of SeP on NAFLD in Korean adults. Also, the number of study participants was relatively small. Another limitation of our study was that we did not perform liver biopsies for the diagnosis of NAFLD. Although liver biopsy is regarded as a gold standard for the diagnosis of NAFLD, it is invasive and associated with morbidities and rare cases of mortality [22]. Furthermore, as histological lesions of NASH are not evenly distributed in the liver, the inherent sampling error of liver biopsies may result in substantial misdiagnosis and staging inaccuracies [35].
- The present study also has several advantages. Using predefined inclusion and exclusion criteria, we enrolled age- and sex-matched individuals from the subjects of a prudently designed cohort study. Also, we used abdominal CT, which is known as the most accurate method for measuring visceral fat. In addition, a diagnosis of NAFLD was defined based on an objective method of averaging LAI in multiple points of liver parenchyma [19].
- In conclusion, the present study demonstrated that novel hepatokine SeP concentrations were increased in subjects with visceral obesity. In addition, circulating SeP levels appear to be significantly associated with cardiovascular risk factors, including subclinical inflammation and arterial stiffness. Furthermore, SeP concentrations were shown to be significantly correlated with LAI and independently associated with NAFLD, even after adjusting for potential confounding factors. These results may warrant further investigation of this novel hepatokine in insulin resistance-related disorders, including metabolic liver diseases.
DISCUSSION
-
Acknowledgements
- Dr. Kyung Mook Choi was supported by the Mid-Career Researcher Program through an NRF grant funded by the Ministry of Education, Science, and Technology, Republic of Korea (No. R01-2007-000-20546-0). Dr. Kyung Mook Choi and Dr. Sei Hyun Baik were supported by the Brain Korea 21 Project of the Ministry of Education and Human Resources Development, Republic of Korea (A102065-1011-1070100).
ACKNOWLEDGMENTS
- 1. Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 2002;346:1221-1231. ArticlePubMed
- 2. Boyko EJ, Fujimoto WY, Leonetti DL, Newell-Morris L. Visceral adiposity and risk of type 2 diabetes: a prospective study among Japanese Americans. Diabetes Care 2000;23:465-471. ArticlePubMedPDF
- 3. Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 2004;114:1752-1761. ArticlePubMedPMC
- 4. Leclercq IA, Da Silva Morais A, Schroyen B, Van Hul N, Geerts A. Insulin resistance in hepatocytes and sinusoidal liver cells: mechanisms and consequences. J Hepatol 2007;47:142-156. ArticlePubMed
- 5. Marra F, Bertolani C. Adipokines in liver diseases. Hepatology 2009;50:957-969. ArticlePubMed
- 6. Vanni E, Bugianesi E, Kotronen A, De Minicis S, Yki-Jarvinen H, Svegliati-Baroni G. From the metabolic syndrome to NAFLD or vice versa? Dig Liver Dis 2010;42:320-330. ArticlePubMed
- 7. Kim SG, Kim HY, Seo JA, Lee KW, Oh JH, Kim NH, Choi KM, Baik SH, Choi DS. Relationship between serum adiponectin concentration, pulse wave velocity and nonalcoholic fatty liver disease. Eur J Endocrinol 2005;152:225-231. ArticlePubMed
- 8. Seo JA, Kim NH, Park SY, Kim HY, Ryu OH, Lee KW, Lee J, Kim DL, Choi KM, Baik SH, Choi DS, Kim SG. Serum retinol-binding protein 4 levels are elevated in non-alcoholic fatty liver disease. Clin Endocrinol (Oxf) 2008;68:555-560. ArticlePubMedPMC
- 9. Stefan N, Hennige AM, Staiger H, Machann J, Schick F, Krober SM, Machicao F, Fritsche A, Haring HU. Alpha2-Heremans-Schmid glycoprotein/fetuin-A is associated with insulin resistance and fat accumulation in the liver in humans. Diabetes Care 2006;29:853-857. PubMed
- 10. Dushay J, Chui PC, Gopalakrishnan GS, Varela-Rey M, Crawley M, Fisher FM, Badman MK, Martinez-Chantar ML, Maratos-Flier E. Increased fibroblast growth factor 21 in obesity and nonalcoholic fatty liver disease. Gastroenterology 2010;139:456-463. ArticlePubMedPMC
- 11. Burk RF, Hill KE. Selenoprotein P: an extracellular protein with unique physical characteristics and a role in selenium homeostasis. Annu Rev Nutr 2005;25:215-235. ArticlePubMed
- 12. Misu H, Takamura T, Takayama H, Hayashi H, Matsuzawa-Nagata N, Kurita S, Ishikura K, Ando H, Takeshita Y, Ota T, Sakurai M, Yamashita T, Mizukoshi E, Honda M, Miyamoto K, Kubota T, Kubota N, Kadowaki T, Kim HJ, Lee IK, Minokoshi Y, Saito Y, Takahashi K, Yamada Y, Takakura N, Kaneko S. A liver-derived secretory protein, selenoprotein P, causes insulin resistance. Cell Metab 2010;12:483-495. ArticlePubMed
- 13. Yang SJ, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Serum selenoprotein P levels in patients with type 2 diabetes and prediabetes: implications for insulin resistance, inflammation, and atherosclerosis. J Clin Endocrinol Metab 2011;96:E1325-E1329. ArticlePubMed
- 14. Zhang Y, Chen X. Reducing selenoprotein P expression suppresses adipocyte differentiation as a result of increased preadipocyte inflammation. Am J Physiol Endocrinol Metab 2011;300:E77-E85. ArticlePubMed
- 15. Kim TN, Yang SJ, Yoo HJ, Lim KI, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence of sarcopenia and sarcopenic obesity in Korean adults: the Korean sarcopenic obesity study. Int J Obes (Lond) 2009;33:885-892. ArticlePubMedPDF
- 16. Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care 2010;33:1497-1499. PubMedPMC
- 17. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J 2002;66:987-992. ArticlePubMed
- 18. Hubscher SG. Histological assessment of non-alcoholic fatty liver disease. Histopathology 2006;49:450-465. ArticlePubMed
- 19. Limanond P, Raman SS, Lassman C, Sayre J, Ghobrial RM, Busuttil RW, Saab S, Lu DS. Macrovesicular hepatic steatosis in living related liver donors: correlation between CT and histologic findings. Radiology 2004;230:276-280. ArticlePubMed
- 20. Yoo HJ, Park MS, Lee CH, Yang SJ, Kim TN, Lim KI, Kang HJ, Song W, Yeon JE, Baik SH, Choi DS, Choi KM. Cutoff points of abdominal obesity indices in screening for non-alcoholic fatty liver disease in Asians. Liver Int 2010;30:1189-1196. ArticlePubMed
- 21. Kim SM, Lee J, Ryu OH, Lee KW, Kim HY, Seo JA, Kim SG, Kim NH, Baik SH, Choi DS, Choi KM. Serum osteoprotegerin levels are associated with inflammation and pulse wave velocity. Clin Endocrinol (Oxf) 2005;63:594-598. ArticlePubMed
- 22. Moore JB. Non-alcoholic fatty liver disease: the hepatic consequence of obesity and the metabolic syndrome. Proc Nutr Soc 2010;69:211-220. ArticlePubMed
- 23. Kantartzis K, Schick F, Haring HU, Stefan N. Environmental and genetic determinants of fatty liver in humans. Dig Dis 2010;28:169-178. ArticlePubMedPDF
- 24. Day CP, James OF. Steatohepatitis: a tale of two "hits"? Gastroenterology 1998;114:842-845. ArticlePubMed
- 25. Hennige AM, Staiger H, Wicke C, Machicao F, Fritsche A, Haring HU, Stefan N. Fetuin-A induces cytokine expression and suppresses adiponectin production. PLoS One 2008;3:e1765ArticlePubMedPMC
- 26. Reinehr T, Roth CL. Fetuin-A and its relation to metabolic syndrome and fatty liver disease in obese children before and after weight loss. J Clin Endocrinol Metab 2008;93:4479-4485. ArticlePubMedPDF
- 27. Zhang X, Yeung DC, Karpisek M, Stejskal D, Zhou ZG, Liu F, Wong RL, Chow WS, Tso AW, Lam KS, Xu A. Serum FGF21 levels are increased in obesity and are independently associated with the metabolic syndrome in humans. Diabetes 2008;57:1246-1253. ArticlePubMedPDF
- 28. Yilmaz Y, Eren F, Yonal O, Kurt R, Aktas B, Celikel CA, Ozdogan O, Imeryuz N, Kalayci C, Avsar E. Increased serum FGF21 levels in patients with nonalcoholic fatty liver disease. Eur J Clin Invest 2010;40:887-892. ArticlePubMed
- 29. Guerrero R, Vega GL, Grundy SM, Browning JD. Ethnic differences in hepatic steatosis: an insulin resistance paradox? Hepatology 2009;49:791-801. ArticlePubMed
- 30. Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, Bertelli C, Fatta E, Bignamini D, Marchesini G, Fargion S. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology 2008;48:792-798. ArticlePubMed
- 31. Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol 2005;25:932-943. ArticlePubMed
- 32. Choi KM, Lee KW, Seo JA, Oh JH, Kim SG, Kim NH, Choi DS, Baik SH. Relationship between brachial-ankle pulse wave velocity and cardiovascular risk factors of the metabolic syndrome. Diabetes Res Clin Pract 2004;66:57-61. ArticlePubMed
- 33. Choi KM, Yoo HJ, Kim HY, Lee KW, Seo JA, Kim SG, Kim NH, Choi DS, Baik SH. Association between endogenous secretory RAGE, inflammatory markers and arterial stiffness. Int J Cardiol 2009;132:96-101. ArticlePubMed
- 34. Blake GJ, Ridker PM. Novel clinical markers of vascular wall inflammation. Circ Res 2001;89:763-771. ArticlePubMed
- 35. Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. LIDO Study Group. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 2005;128:1898-1906. ArticlePubMed
REFERENCES

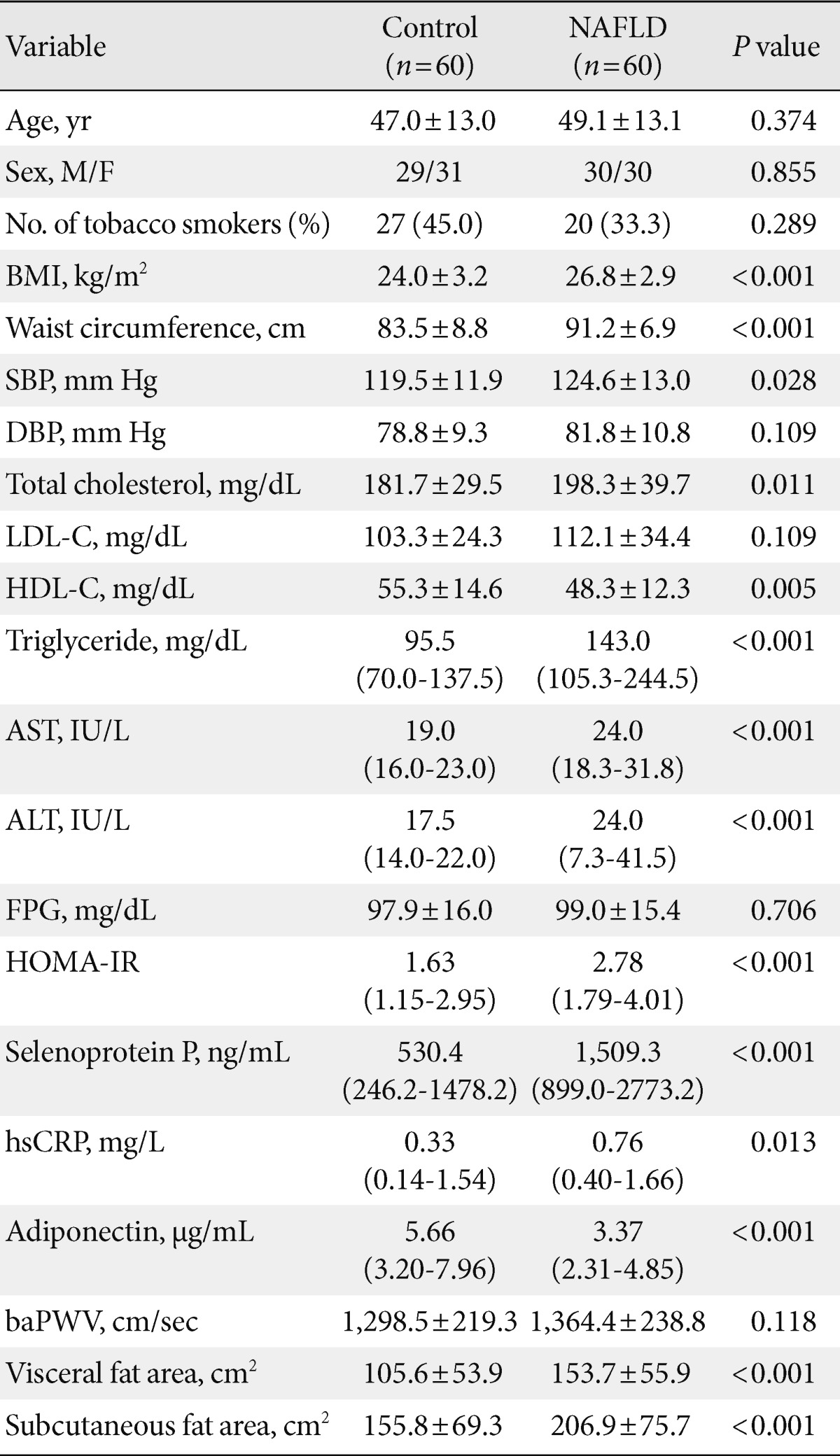
Values are presented as mean±standard deviation, median (interquartile range), or number (%). P values were calculated using an independent two-sample t-test or the Mann-Whitney U test.
NAFLD, nonalcoholic fatty liver disease; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; FPG, fasting plasma glucose; HOMA-IR, homeostasis model assessment of insulin resistance; hsCRP, high sensitivity C-reactive protein; baPWV, brachial-ankle pulse wave velocity.
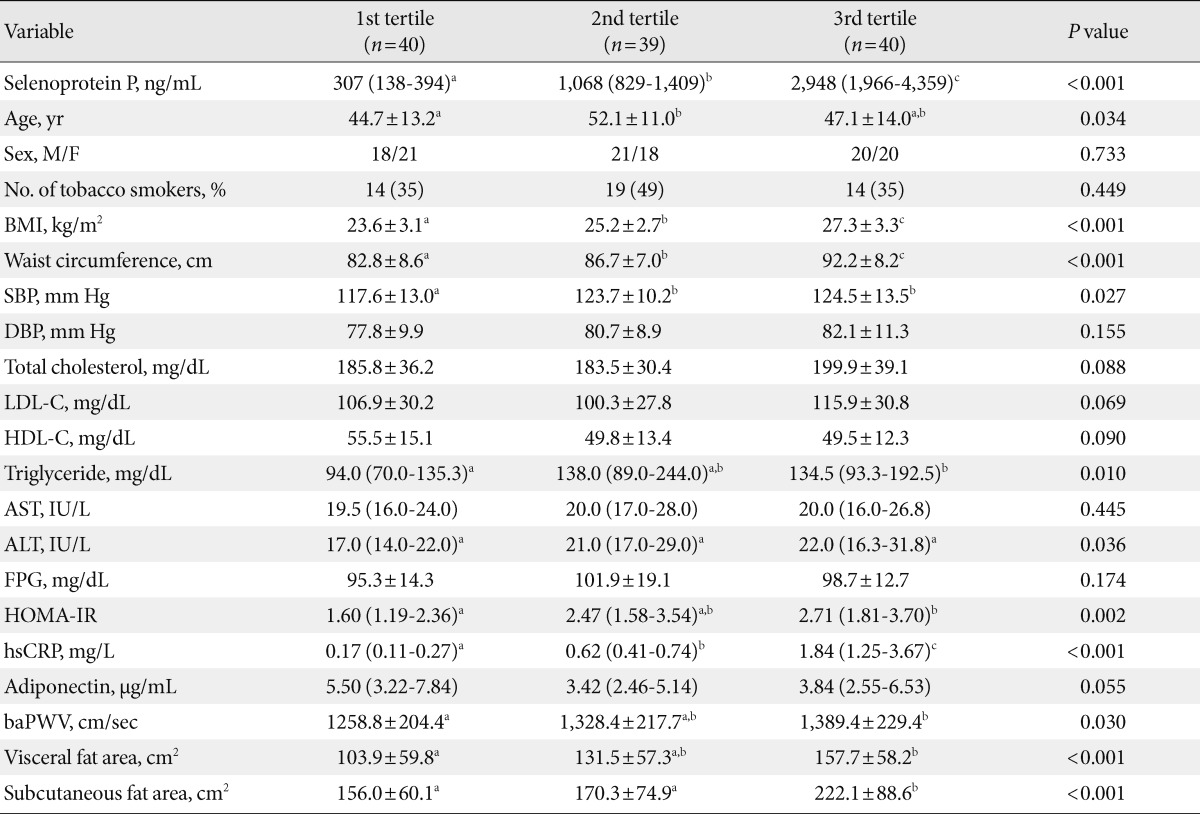
Values are presented as mean±standard deviation, median (interquartile range), or number (%). P values represent overall differences across groups as determined by (nonparametric) ANOVA for continuous variables and Fisher's exact test or Pearson's chi-squared test for categorical variables.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; FPG, fasting plasma glucose; HOMA-IR, homeostasis model assessment of insulin resistance; hsCRP, high sensitivity C-reactive protein; baPWV, brachial-ankle pulse wave velocity.
a,b,cSame letters indicate no statistical significance based on Tukey's HSD post-hoc test and the Bonferroni correction.
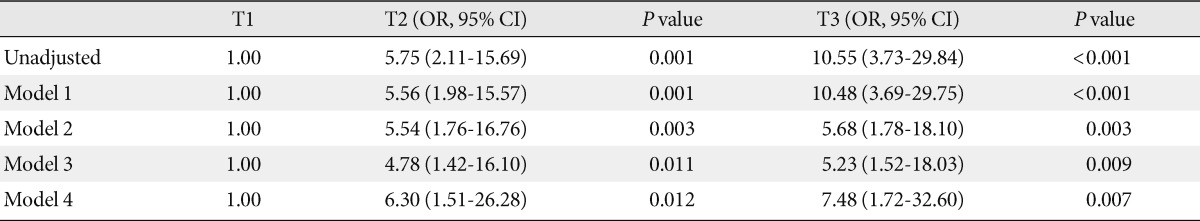
Model 1: adjusted for age, sex; Model 2: adjusted for age, sex, body mass index (BMI), and smoking status; Model 3: adjusted for age, sex, BMI, smoking status, systolic blood pressure (SBP), diastolic blood pressure (DBP), triglycerides, and high density lipoprotein cholesterol (HDL-C) values; Model 4: adjusted for age, sex, BMI, smoking status, SBP, DBP, triglycerides, HDL-C, high sensitivity C-reactive protein, adiponectin, and homeostasis model assessment of insulin resistance values.
OR, odds ratio; CI, confidence interval.
Figure & Data
References
Citations

- Myosteatosis: Diagnosis, pathophysiology and consequences in metabolic dysfunction-associated steatotic liver disease
Guillaume Henin, Audrey Loumaye, Isabelle A. Leclercq, Nicolas Lanthier
JHEP Reports.2024; 6(2): 100963. CrossRef - Association between serum trace element, mineral, and amino acid levels with non-alcoholic fatty liver disease (NAFLD) in adult women
Alexey A. Tinkov, Tatiana V. Korobeinikova, Galina D. Morozova, Michael Aschner, Daria V. Mak, Abel Santamaria, Joao B.T. Rocha, Tatiana I. Sotnikova, Serafima Ia. Tazina, Anatoly V. Skalny
Journal of Trace Elements in Medicine and Biology.2024; 83: 127397. CrossRef - Adipose-derived extracellular vesicles – a novel cross-talk mechanism in insulin resistance, non-alcoholic fatty liver disease, and polycystic ovary syndrome
Dušan Mladenović, Milena Vesković, Nikola Šutulović, Dragan Hrnčić, Olivera Stanojlović, Lena Radić, Jelica Bjekić Macut, Djuro Macut
Endocrine.2024;[Epub] CrossRef - Association of metabolic-dysfunction associated steatotic liver disease with polycystic ovary syndrome
Qiuyu Xu, Jie Zhang, Yan Lu, Ling Wu
iScience.2024; 27(2): 108783. CrossRef - The role of hepatokines in NAFLD
Norbert Stefan, Fritz Schick, Andreas L. Birkenfeld, Hans-Ulrich Häring, Morris F. White
Cell Metabolism.2023; 35(2): 236. CrossRef - The regulatory role of metabolic organ-secreted factors in the nonalcoholic fatty liver disease and cardiovascular disease
Li Qin, Junru Wu, Xuejing Sun, Xuewei Huang, Wei Huang, Chunyan Weng, Jingjing Cai
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - The Role of Organokines in Obesity and Type 2 Diabetes and Their Functions as Molecular Transducers of Nutrition and Exercise
Ji Ye Lim, Eunju Kim
Metabolites.2023; 13(9): 979. CrossRef - Hepatokine Profile in Adolescents with Polycystic Ovary Syndrome: A Case–Control Study
Aikaterini Giannouli, Charikleia Stefanaki, Christos Kouskoutis, Marianna Konidari, Iliana Mani, Konstantina Konidari, Sophia L. Markantonis, Aimilia Mantzou, Spyridon P. Dourakis, Efthymios Deligeoroglou, Flora Bacopoulou
Journal of Clinical Medicine.2023; 12(17): 5744. CrossRef - The Interconnection between Hepatic Insulin Resistance and Metabolic Dysfunction-Associated Steatotic Liver Disease—The Transition from an Adipocentric to Liver-Centric Approach
Milena Vesković, Nikola Šutulović, Dragan Hrnčić, Olivera Stanojlović, Djuro Macut, Dušan Mladenović
Current Issues in Molecular Biology.2023; 45(11): 9084. CrossRef - Sulforaphane decreases serum selenoprotein P levels through enhancement of lysosomal degradation independent of Nrf2
Xinying Ye, Takashi Toyama, Keiko Taguchi, Kotoko Arisawa, Takayuki Kaneko, Ryouhei Tsutsumi, Masayuki Yamamoto, Yoshiro Saito
Communications Biology.2023;[Epub] CrossRef - “Alphabet” Selenoproteins: Implications in Pathology
Carmen Beatrice Dogaru, Carmen Duță, Corina Muscurel, Irina Stoian
International Journal of Molecular Sciences.2023; 24(20): 15344. CrossRef - Metabolic dysfunction-associated steatotic liver disease and the heart
Stan Driessen, Sven M. Francque, Stefan D. Anker, Manuel Castro Cabezas, Diederick E. Grobbee, Maarten E. Tushuizen, Adriaan G. Holleboom
Hepatology.2023;[Epub] CrossRef - Associations between Circulating SELENOP Level and Disorders of Glucose and Lipid Metabolism: A Meta-Analysis
Ruirui Yu, Zhoutian Wang, Miaomiao Ma, Ping Xu, Longjian Liu, Alexey A. Tinkov, Xin Gen Lei, Ji-Chang Zhou
Antioxidants.2022; 11(7): 1263. CrossRef - Contribution of organokines in the development of NAFLD/NASH associated hepatocellular carcinoma
Meenakshi Vachher, Savita Bansal, Bhupender Kumar, Sandeep Yadav, Taruna Arora, Nalini Moza Wali, Archana Burman
Journal of Cellular Biochemistry.2022; 123(10): 1553. CrossRef - Regulatory network and interplay of hepatokines, stellakines, myokines and adipokines in nonalcoholic fatty liver diseases and nonalcoholic steatohepatitis
Bing Yang, Liqing Lu, Dongmei Zhou, Wei Fan, Lucía Barbier-Torres, Justin Steggerda, Heping Yang, Xi Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Cytokines and regulation of glucose and lipid metabolism in the obesity
V. I. Scherbakov, G. A. Skosyreva, T. I. Ryabichenko, O. O. Obukhova
Obesity and metabolism.2022; 19(3): 317. CrossRef - SeP is elevated in NAFLD and participates in NAFLD pathogenesis through AMPK/ACC pathway
Yi Chen, Xinjue He, Xueyang Chen, Youming Li, Yini Ke
Journal of Cellular Physiology.2021; 236(5): 3800. CrossRef - Hepatokines and metabolism: Deciphering communication from the liver
Sharon O. Jensen-Cody, Matthew J. Potthoff
Molecular Metabolism.2021; 44: 101138. CrossRef - Weight-loss-independent benefits of exercise on liver steatosis and stiffness in Japanese men with NAFLD
Sechang Oh, Takehiko Tsujimoto, Bokun Kim, Fumihiko Uchida, Hideo Suzuki, Seiichiro Iizumi, Tomonori Isobe, Takeji Sakae, Kiyoji Tanaka, Junichi Shoda
JHEP Reports.2021; 3(3): 100253. CrossRef - Efficacy of Weight Reduction on Pediatric Nonalcoholic Fatty Liver Disease: Opportunities to Improve Treatment Outcomes Through Pharmacotherapy
Chance S. Friesen, Chelsea Hosey-Cojocari, Sherwin S. Chan, Iván L. Csanaky, Jonathan B. Wagner, Brooke R. Sweeney, Alec Friesen, Jason D. Fraser, Valentina Shakhnovich
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of Urinary and Dietary Selenium and of Serum Selenium Species with Serum Alanine Aminotransferase in a Healthy Italian Population
Teresa Urbano, Tommaso Filippini, Daniela Lasagni, Tiziana De Luca, Peter Grill, Sabrina Sucato, Elisa Polledri, Guy Djeukeu Noumbi, Marcella Malavolti, Annalisa Santachiara, Thelma A. Pertinhez, Roberto Baricchi, Silvia Fustinoni, Bernhard Michalke, Marc
Antioxidants.2021; 10(10): 1516. CrossRef - Selenotranscriptome Network in Non-alcoholic Fatty Liver Disease
Kaitlin Day, Lucia A. Seale, Ross M. Graham, Barbara R. Cardoso
Frontiers in Nutrition.2021;[Epub] CrossRef - Hepatokines and Non-Alcoholic Fatty Liver Disease: Linking Liver Pathophysiology to Metabolism
Tae Hyun Kim, Dong-Gyun Hong, Yoon Mee Yang
Biomedicines.2021; 9(12): 1903. CrossRef - Leukocyte cell-derived chemotaxin-2 and fibroblast growth factor 21 in alcohol-induced liver cirrhosis
Jarosław Jerzy Sak, Andrzej Prystupa, Paweł Kiciński, Dorota Luchowska-Kocot, Ewa Kurys-Denis, Hanna Bis-Wencel
World Journal of Hepatology.2021; 13(12): 2071. CrossRef - Acute Hyperenergetic, High-Fat Feeding Increases Circulating FGF21, LECT2, and Fetuin-A in Healthy Men
Scott A Willis, Jack A Sargeant, Thomas Yates, Toshinari Takamura, Hiroaki Takayama, Vinay Gupta, Emily Brittain, Joe Crawford, Siôn A Parry, Alice E Thackray, Veronica Varela-Mato, David J Stensel, Rachel M Woods, Carl J Hulston, Guruprasad P Aithal, Jam
The Journal of Nutrition.2020; 150(5): 1076. CrossRef - Targeting fibrinogen‐like protein 1 is a novel therapeutic strategy to combat obesity
Hung‐Tsung Wu, Szu‐Chi Chen, Kang‐Chih Fan, Chun‐Heng Kuo, Shin‐Yu Lin, Shu‐Huei Wang, Chih‐Jen Chang, Hung‐Yuan Li
The FASEB Journal.2020; 34(2): 2958. CrossRef - Nonalcoholic fatty liver disease and cardiovascular disease phenotypes
Giandomenico Bisaccia, Fabrizio Ricci, Cesare Mantini, Claudio Tana, Gian Luca Romani, Cosima Schiavone, Sabina Gallina
SAGE Open Medicine.2020; 8: 205031212093380. CrossRef - Higher Serum Selenoprotein P Level as a Novel Inductor of Metabolic Complications in Psoriasis
Anna Baran, Julia Nowowiejska, Julita Anna Krahel, Tomasz W. Kaminski, Magdalena Maciaszek, Iwona Flisiak
International Journal of Molecular Sciences.2020; 21(13): 4594. CrossRef - The Role of Exercise in the Interplay between Myokines, Hepatokines, Osteokines, Adipokines, and Modulation of Inflammation for Energy Substrate Redistribution and Fat Mass Loss: A Review
Adrian M. Gonzalez-Gil, Leticia Elizondo-Montemayor
Nutrients.2020; 12(6): 1899. CrossRef - Selenoprotein P; P for Plasma, Prognosis, Prophylaxis, and More
Ryouhei Tsutsumi, Yoshiro Saito
Biological and Pharmaceutical Bulletin.2020; 43(3): 366. CrossRef - Selenium and selenoprotein P in nonalcoholic fatty liver disease
Stergios A. Polyzos, Jannis Kountouras, Antonis Goulas, Leonidas Duntas
Hormones.2020; 19(1): 61. CrossRef - The Effects of Endoplasmic-Reticulum-Resident Selenoproteins in a Nonalcoholic Fatty Liver Disease Pig Model Induced by a High-Fat Diet
Pengzu Wang, Zhuang Lu, Meng He, Baoming Shi, Xingen Lei, Anshan Shan
Nutrients.2020; 12(3): 692. CrossRef - The risk of pregnancy‐associated hypertension in women with nonalcoholic fatty liver disease
Young Mi Jung, Seung Mi Lee, Subeen Hong, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan‐Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Liver International.2020; 40(10): 2417. CrossRef - Why Multiples of 21? Why does Selenoprotein P Contain Multiple Selenocysteine Residues?
Janinah Baclaocos, John James Mackrill
Current Nutraceuticals.2020; 1(1): 42. CrossRef - Selenium and Selenoproteins in Adipose Tissue Physiology and Obesity
Alexey A. Tinkov, Olga P. Ajsuvakova, Tommaso Filippini, Ji-Chang Zhou, Xin Gen Lei, Eugenia R. Gatiatulina, Bernhard Michalke, Margarita G. Skalnaya, Marco Vinceti, Michael Aschner, Anatoly V. Skalny
Biomolecules.2020; 10(4): 658. CrossRef - Metabolic adaptations after bariatric surgery: adipokines, myokines and hepatokines
Justine Faramia, Giada Ostinelli, Virginie Drolet-Labelle, Frédéric Picard, André Tchernof
Current Opinion in Pharmacology.2020; 52: 67. CrossRef - Physiopathology of Lifestyle Interventions in Non-Alcoholic Fatty Liver Disease (NAFLD)
David Carneros, Guillermo López-Lluch, Matilde Bustos
Nutrients.2020; 12(11): 3472. CrossRef - Interplay between Oxidative Stress and Metabolic Derangements in Non-Alcoholic Fatty Liver Disease: The Role of Selenoprotein P
Gian Paolo Caviglia, Chiara Rosso, Angelo Armandi, Melania Gaggini, Fabrizia Carli, Maria Lorena Abate, Antonella Olivero, Davide Giuseppe Ribaldone, Giorgio Maria Saracco, Amalia Gastaldelli, Elisabetta Bugianesi
International Journal of Molecular Sciences.2020; 21(22): 8838. CrossRef - Can hepatokines be regarded as novel non-invasive serum biomarkers of intrahepatic lipid content in obese children?
Marta Flisiak-Jackiewicz, Anna Bobrus-Chociej, Natalia Wasilewska, Eugeniusz Tarasow, Malgorzata Wojtkowska, Dariusz Marek Lebensztejn
Advances in Medical Sciences.2019; 64(2): 280. CrossRef - Dietary pattern associated with selenoprotein P and MRI-derived body fat volumes, liver signal intensity, and metabolic disorders
Romina di Giuseppe, Sandra Plachta-Danielzik, Manja Koch, Ute Nöthlings, Sabrina Schlesinger, Jan Borggrefe, Marcus Both, Hans-Peter Müller, Jan Kassubek, Gunnar Jacobs, Wolfgang Lieb
European Journal of Nutrition.2019; 58(3): 1067. CrossRef - Cytokines and Abnormal Glucose and Lipid Metabolism
Jie Shi, Jiangao Fan, Qing Su, Zhen Yang
Frontiers in Endocrinology.2019;[Epub] CrossRef - Role of exercise-induced hepatokines in metabolic disorders
Gaël Ennequin, Pascal Sirvent, Martin Whitham
American Journal of Physiology-Endocrinology and Metabolism.2019; 317(1): E11. CrossRef - Metabolomics signature associated with circulating serum selenoprotein P levels
Romina di Giuseppe, Manja Koch, Ute Nöthlings, Gabi Kastenmüller, Anna Artati, Jerzy Adamski, Gunnar Jacobs, Wolfgang Lieb
Endocrine.2019; 64(3): 486. CrossRef - Secretomics to Discover Regulators in Diseases
Parkyong Song, Yonghoon Kwon, Jae-Yeol Joo, Do-Geun Kim, Jong Hyuk Yoon
International Journal of Molecular Sciences.2019; 20(16): 3893. CrossRef - Impact of Lipotoxicity on Tissue “Cross Talk” and Metabolic Regulation
Magdalene K. Montgomery, William De Nardo, Matthew J. Watt
Physiology.2019; 34(2): 134. CrossRef - The Liver as an Endocrine Organ—Linking NAFLD and Insulin Resistance
Matthew J Watt, Paula M Miotto, William De Nardo, Magdalene K Montgomery
Endocrine Reviews.2019; 40(5): 1367. CrossRef - Inter-organ cross-talk in metabolic syndrome
Christina Priest, Peter Tontonoz
Nature Metabolism.2019; 1(12): 1177. CrossRef - Serum selenoprotein P, but not selenium, predicts future hyperglycemia in a general Japanese population
Swe Mar Oo, Hirofumi Misu, Yoshiro Saito, Mutsumi Tanaka, Seiji Kato, Yuki Kita, Hiroaki Takayama, Yumie Takeshita, Takehiro Kanamori, Toru Nagano, Masatoshi Nakagen, Takeshi Urabe, Naoto Matsuyama, Shuichi Kaneko, Toshinari Takamura
Scientific Reports.2018;[Epub] CrossRef - NAFLD and cardiovascular disease
Elisabete Martins, Ana Oliveira
Porto Biomedical Journal.2018; 3(2): e2. CrossRef - The influence of adiposity and acute exercise on circulating hepatokines in normal-weight and overweight/obese men
Jack A. Sargeant, Guruprasad P. Aithal, Toshinari Takamura, Hirofumi Misu, Hiroaki Takayama, Jessica A. Douglas, Mark C. Turner, David J. Stensel, Myra A. Nimmo, David R. Webb, Thomas Yates, James A. King
Applied Physiology, Nutrition, and Metabolism.2018; 43(5): 482. CrossRef - Low Urine pH Is Associated with Non-alcoholic Fatty Liver Disease: A Community-based Cross-sectional Study
Teruki Miyake, Sakiko Yoshida, Shin Yamamoto, Shinya Furukawa, Osamu Yoshida, Sayaka Kanzaki, Hidenori Senba, Toru Ishihara, Mitsuhito Koizumi, Yoshio Tokumoto, Masashi Hirooka, Teru Kumagi, Masanori Abe, Kohichiro Kitai, Bunzo Matsuura, Yoichi Hiasa
Internal Medicine.2018; 57(19): 2799. CrossRef - Evaluation of endothelial dysfunction in patients with nonalcoholic fatty liver disease: Association of selenoprotein P with carotid intima-media thickness and endothelium-dependent vasodilation
Ibrahim Cetindağlı, Muammer Kara, Alpaslan Tanoglu, Veysel Ozalper, Serkan Aribal, Yusuf Hancerli, Mehmet Unal, Onur Ozarı, Serdar Hira, Mustafa Kaplan, Yusuf Yazgan
Clinics and Research in Hepatology and Gastroenterology.2017; 41(5): 516. CrossRef - Differences in the risk of fatty liver for onset of impaired fasting glucose according to baseline plasma glucose levels
Teruki Miyake, Masashi Hirooka, Osamu Yoshida, Shinya Furukawa, Teru Kumagi, Mitsuhito Koizumi, Shin Yamamoto, Taira Kuroda, Eiji Arimitsu, Eiji Takeshita, Masanori Abe, Kohichiro Kitai, Bunzo Matsuura, Yoichi Hiasa
Journal of Gastroenterology.2017; 52(2): 237. CrossRef - Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance
Ruth C. R. Meex, Matthew J. Watt
Nature Reviews Endocrinology.2017; 13(9): 509. CrossRef - Circulating selenoprotein P levels in relation to MRI‐derived body fat volumes, liver fat content, and metabolic disorders
Romina di Giuseppe, Manja Koch, Sabrina Schlesinger, Jan Borggrefe, Marcus Both, Hans‐Peter Müller, Jan Kassubek, Gunnar Jacobs, Ute Nöthlings, Wolfgang Lieb
Obesity.2017; 25(6): 1128. CrossRef - Eicosapentaenoic acid down-regulates expression of the selenoprotein P gene by inhibiting SREBP-1c protein independently of the AMP-activated protein kinase pathway in H4IIEC3 hepatocytes
Natsumi Tajima-Shirasaki, Kiyo-aki Ishii, Hiroaki Takayama, Takayoshi Shirasaki, Hisakazu Iwama, Keita Chikamoto, Yoshiro Saito, Yasumasa Iwasaki, Atsushi Teraguchi, Fei Lan, Akihiro Kikuchi, Yumie Takeshita, Koji Murao, Seiichi Matsugo, Shuichi Kaneko, H
Journal of Biological Chemistry.2017; 292(26): 10791. CrossRef - Selenoprotein P is elevated in individuals with obesity, but is not independently associated with insulin resistance
Miaoxin Chen, Bo Liu, David Wilkinson, Amy T. Hutchison, Campbell H. Thompson, Gary A. Wittert, Leonie K. Heilbronn
Obesity Research & Clinical Practice.2017; 11(2): 227. CrossRef - Cardiovascular Risk in Patients with Non-alcoholic Fatty Liver Disease
Hak Soo Kim, Yong Kyun Cho
The Korean Journal of Gastroenterology.2017; 69(6): 333. CrossRef - Association between betatrophin/ANGPTL8 and non-alcoholic fatty liver disease: animal and human studies
Yong-ho Lee, Sang-Guk Lee, Chan Joo Lee, Soo Hyun Kim, Young-Mi Song, Mi Ra Yoon, Byung Hun Jeon, Jae Hyuk Lee, Byung-Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong-Soo Cha
Scientific Reports.2016;[Epub] CrossRef - Implication of hepatokines in metabolic disorders and cardiovascular diseases
Tae Woo Jung, Hye Jin Yoo, Kyung Mook Choi
BBA Clinical.2016; 5: 108. CrossRef - Selenoproteins: Antioxidant selenoenzymes and beyond
Holger Steinbrenner, Bodo Speckmann, Lars-Oliver Klotz
Archives of Biochemistry and Biophysics.2016; 595: 113. CrossRef - Metabolic Adaptation in Obesity and Type II Diabetes: Myokines, Adipokines and Hepatokines
Kyoung-Jin Oh, Da Lee, Won Kim, Baek Han, Sang Lee, Kwang-Hee Bae
International Journal of Molecular Sciences.2016; 18(1): 8. CrossRef - Pathogenesis of nonalcoholic steatohepatitis
Wensheng Liu, Robert D. Baker, Tavleen Bhatia, Lixin Zhu, Susan S. Baker
Cellular and Molecular Life Sciences.2016; 73(10): 1969. CrossRef - Stéatose et résistance à l’insuline : implication des hépatokines
C. Bertrand, P. Valet, I. Castan-Laurell
Obésité.2016; 11(3): 170. CrossRef - Pathophysiology of Non Alcoholic Fatty Liver Disease
Salvatore Petta, Amalia Gastaldelli, Eleni Rebelos, Elisabetta Bugianesi, Piergiorgio Messa, Luca Miele, Gianluca Svegliati-Baroni, Luca Valenti, Ferruccio Bonino
International Journal of Molecular Sciences.2016; 17(12): 2082. CrossRef - Alterations in serum levels of fetuin A and selenoprotein P in chronic hepatitis C patients with concomitant type 2 diabetes: A case-control study
Sahar A. Ali, Walaa M.H. Nassif, Dalia H.A. Abdelaziz
Clinics and Research in Hepatology and Gastroenterology.2016; 40(4): 465. CrossRef - Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications
Sven M. Francque, Denise van der Graaff, Wilhelmus J. Kwanten
Journal of Hepatology.2016; 65(2): 425. CrossRef - “Omics” of Selenium Biology: A Prospective Study of Plasma Proteome Network Before and After Selenized-Yeast Supplementation in Healthy Men
Indu Sinha, Kubra Karagoz, Rachel L. Fogle, Christopher S. Hollenbeak, Arnold H. Zea, Kazim Y. Arga, Anne E. Stanley, Wayne C. Hawkes, Raghu Sinha
OMICS: A Journal of Integrative Biology.2016; 20(4): 202. CrossRef - Nonalcoholic steatohepatitis is strongly associated with sarcopenic obesity in patients with cirrhosis undergoing liver transplant evaluation
Sandra Carias, Ana Lia Castellanos, Valery Vilchez, Rashmi Nair, Anna Christina Dela Cruz, Jennifer Watkins, Terrence Barrett, Patel Trushar, Karyn Esser, Roberto Gedaly
Journal of Gastroenterology and Hepatology.2016; 31(3): 628. CrossRef - Variants in Genes Controlling Oxidative Metabolism Contribute to Lower Hepatic ATP Independent of Liver Fat Content in Type 1 Diabetes
Sofiya Gancheva, Alessandra Bierwagen, Kirti Kaul, Christian Herder, Peter Nowotny, Sabine Kahl, Guido Giani, Birgit Klueppelholz, Birgit Knebel, Paul Begovatz, Klaus Strassburger, Hadi Al-Hasani, Jesper Lundbom, Julia Szendroedi, Michael Roden
Diabetes.2016; 65(7): 1849. CrossRef - Selenoprotein P is not elevated in gestational diabetes mellitus
Alev E. Altinova, Ozlem T. Iyidir, Cigdem Ozkan, Damla Ors, Merve Ozturk, Ozlem Gulbahar, Nuray Bozkurt, Fusun B. Toruner, Mujde Akturk, Nuri Cakir, Metin Arslan
Gynecological Endocrinology.2015; 31(11): 874. CrossRef - Selenium and Human Health: Witnessing a Copernican Revolution?
Ewa Jablonska, Marco Vinceti
Journal of Environmental Science and Health, Part C.2015; 33(3): 328. CrossRef - Toenail selenium and risk of type 2 diabetes: the ORDET cohort study
Marco Vinceti, Sara Grioni, Dorothea Alber, Dario Consonni, Carlotta Malagoli, Claudia Agnoli, Marcella Malavolti, Valeria Pala, Vittorio Krogh, Sabina Sieri
Journal of Trace Elements in Medicine and Biology.2015; 29: 145. CrossRef - Expression of Selenoprotein Genes Is Affected by Obesity of Pigs Fed a High-Fat Diet
Hua Zhao, Ke Li, Jia-Yong Tang, Ji-Chang Zhou, Kang-Ning Wang, Xin-Jie Xia, Xin Gen Lei
The Journal of Nutrition.2015; 145(7): 1394. CrossRef - Hepatokines as a Link between Obesity and Cardiovascular Diseases
Hye Jin Yoo, Kyung Mook Choi
Diabetes & Metabolism Journal.2015; 39(1): 10. CrossRef - The Dipeptidyl Peptidase-4 Inhibitor Teneligliptin Attenuates Hepatic Lipogenesis via AMPK Activation in Non-Alcoholic Fatty Liver Disease Model Mice
Takayasu Ideta, Yohei Shirakami, Tsuneyuki Miyazaki, Takahiro Kochi, Hiroyasu Sakai, Hisataka Moriwaki, Masahito Shimizu
International Journal of Molecular Sciences.2015; 16(12): 29207. CrossRef - Dietary selenate attenuates adiposity and improves insulin sensitivity in high-fat diet-induced obese mice
Choon Young Kim, Yuyan Zhu, Kimberly K. Buhman, Kee-Hong Kim
Journal of Functional Foods.2015; 17: 33. CrossRef - Use of a Diabetes Self-Assessment Score to Predict Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis
Gyuri Kim, Yong-ho Lee, Young Min Park, Jungghi Kim, Heesuk Kim, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Dae Jung Kim
Medicine.2015; 94(27): e1103. CrossRef - Inhibition of SH2-domain-containing inositol 5-phosphatase (SHIP2) ameliorates palmitate induced-apoptosis through regulating Akt/FOXO1 pathway and ROS production in HepG2 cells
Sattar Gorgani-Firuzjaee, Khosrow Adeli, Reza Meshkani
Biochemical and Biophysical Research Communications.2015; 464(2): 441. CrossRef - Exendin-4 Inhibits the Expression of SEPP1 and Fetuin-A via Improvement of Palmitic Acid-Induced Endoplasmic Reticulum Stress by AMPK
Jinmi Lee, Seok-Woo Hong, Se Eun Park, Eun-Jung Rhee, Cheol-Young Park, Ki-Won Oh, Sung-Woo Park, Won-Young Lee
Endocrinology and Metabolism.2015; 30(2): 177. CrossRef - AMPK activator-mediated inhibition of endoplasmic reticulum stress ameliorates carrageenan-induced insulin resistance through the suppression of selenoprotein P in HepG2 hepatocytes
Tae Woo Jung, So Young Lee, Ho Cheol Hong, Hae Yoon Choi, Hye Jin Yoo, Sei Hyun Baik, Kyung Mook Choi
Molecular and Cellular Endocrinology.2014; 382(1): 66. CrossRef - HIF‐1α Expression as a Protective Strategy of HepG2 Cells Against Fatty Acid‐Induced Toxicity
Wonbaek Yoo, Kyung Hee Noh, Jae Hee Ahn, Ji Hee Yu, Ji A. Seo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Tae Woo Kim, Hyo Joon Kim, Nan Hee Kim
Journal of Cellular Biochemistry.2014; 115(6): 1147. CrossRef - Genetic variants in selenoprotein P plasma 1 gene (SEPP1) are associated with fasting insulin and first phase insulin response in Hispanics
Jacklyn N. Hellwege, Nicholette D. Palmer, Julie T. Ziegler, Carl D. Langefeld, Carlos Lorenzo, Jill M. Norris, Toshinari Takamura, Donald W. Bowden
Gene.2014; 534(1): 33. CrossRef - Levels of circulating selenoprotein P, fibroblast growth factor (FGF) 21 and FGF23 in relation to the metabolic syndrome in young children
B-J Ko, S M Kim, K H Park, H S Park, C S Mantzoros
International Journal of Obesity.2014; 38(12): 1497. CrossRef - The association between non-alcoholic fatty liver disease and carotid atherosclerosis in subjects with within-reference range alanine aminotransferase levels
Kyung-Soo Kim, Hyun-Ju Oh, Dae-Jung Kim, Soo-Kyung Kim, Seok Won Park, Yong-Wook Cho, Kap-Bum Huh
Endocrine Journal.2013; 60(12): 1295. CrossRef

 KDA
KDA PubReader
PubReader Cite
Cite




