
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- Others
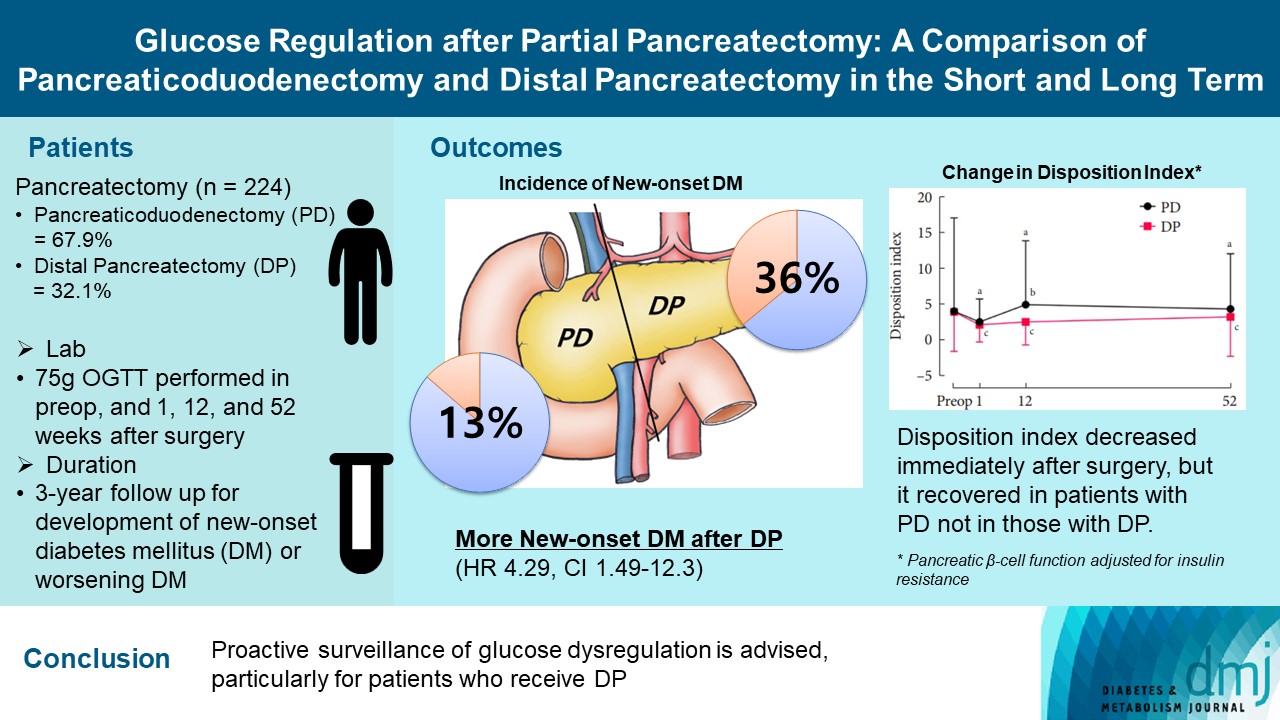
- Glucose Regulation after Partial Pancreatectomy: A Comparison of Pancreaticoduodenectomy and Distal Pancreatectomy in the Short and Long Term
- Jun Suh Lee, Minji Sohn, Kyuho Kim, Yoo-Seok Yoon, Soo Lim
- Diabetes Metab J. 2023;47(5):703-714. Published online June 22, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0205
- 1,752 View
- 153 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Long term quality of life is becoming increasingly crucial as survival following partial pancreatectomy rises. The purpose of this study was to investigate the difference in glucose dysregulation after pancreaticoduodenectomy (PD) or distal pancreatectomy (DP).
Methods
In this prospective observational study from 2015 to 2018, 224 patients who underwent partial pancreatectomy were selected: 152 (67.9%) received PD and 72 (32.1%) received DP. Comprehensive assessment for glucose regulation, including a 75 g oral glucose tolerance test was conducted preoperatively, and 1, 12, and 52 weeks after surgery. Patients were further monitored up to 3 years to investigate development of new-onset diabetes mellitus (NODM) in patients without diabetes mellitus (DM) at baseline or worsening of glucose regulation (≥1% increase in glycosylated hemoglobin [HbA1c]) in those with preexisting DM.
Results
The disposition index, an integrated measure of β-cell function, decreased 1 week after surgery in both groups, but it increased more than baseline level in the PD group while its decreased level was maintained in the DP group, resulting in a between-group difference at the 1-year examination (P<0.001). During follow-up, the DP group showed higher incidence of NODM and worsening of glucose regulation than the PD group with hazard ratio (HR) 4.29 (95% confidence interval [CI], 1.49 to 12.3) and HR 2.15 (95% CI, 1.09 to 4.24), respectively, in the multivariate analysis including dynamic glycemic excursion profile. In the DP procedure, distal DP and spleen preservation were associated with better glucose regulation. DP had a stronger association with glucose dysregulation than PD.
Conclusion
Proactive surveillance of glucose dysregulation is advised, particularly for patients who receive DP.
- AICAR Reversed the Glucolipotoxicity Induced beta-cell Dysfunction through Suppression of PPAR-gamma-coactivator-1 (PGC-1) Overexpression.
- Hyuk Sang Kwon, Ji Won Kim, Heon Seok Park, Seung Hyun Ko, Bong Yun Cha, Ho Young Son, Kun Ho Yoon
- Korean Diabetes J. 2007;31(4):310-318. Published online July 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.4.310
- 2,034 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Glucolipotoxicity plays an important role in the progression of type 2 diabetes mellitus via inducing insulin secretory dysfunction. Expression of insulin gene in pancreatic beta cell might be regulated by AMP-activated protein kinase (AMPK), which is recognized as a key molecule of energy metabolism. We studied the effects of AMPK on glucolipotoxicity-induced beta-cell dysfunction by suppression of PPAR-gamma-coactivator-1 (PGC-1) in vitro and in vivo. Method: Glucolipotoxicity was induced by 33.3 mM glucose and 0.6 mM (palmitate and oleate) for 3 days in isolated rat islets. Messenger RNA (mRNA) expressions of beta-cell specific gene like insulin, BETA2/NeuroD and PGC-1 induced by glucolipotoxic condition and their changes with 5-aminoimidazole-4-carboxy-amide-1-D-ribofuranoside (AICAR) treatment were investigated using RT-PCR. We also examined glucose stimulated insulin secretion in same conditions. Furthermore, SD rats were submitted to a 90% partial pancreatectomy (Px) and randomized into two groups; Ad-GFP-infected Px rats (n = 3) and Ad-siPGC- 1-infected Px rats (n = 3). Then, the Px rats were infected with Ad-GFP or Ad-siPGC-1 (1 x 10(9) pfu) via celiac artery. After 12 days of viral infection, we measured body weight and performed the intraperitoneal glucose tolerance test (IP-GTT). RESULTS: Glucolipotoxicity resulted in blunting of glucose-stimulated insulin secretion, which was recovered by the AICAR treatment in vitro. Suppression in their expressions of insulin and BETA2/NeuroD gene by glucolipotoxic condition were improved with AICAR treatment. However, PGC-1alpha expression was gradually increased by glucolipotoxicity, and suppressed by AICAR treatment. Overexpression of PGC-1 using an adenoviral vector in freshly isolated rat islets suppressed insulin gene expression. We also confirmed the function of PGC-1 using an Ad-siPGC-1 in vivo. Direct infection of Ad-siPGC-1 in 90% pancreatectomized rats significantly improved glucose tolerance and increased body weight. CONCLUSION: AMPK could protect against glucolipotoxicity induced beta-cell dysfunction and the suppression of PGC-1 gene expression might involved in the insulin regulatory mechanism by AMPK.
- Proliferation and Differentiation of Pancreatic beta Cells in L-type Calcium Channel alpha(1D) Subunit (Ca(v)1.3) Heterozygous Knock Out Mice After Partial Pancreatectomy.
- Yoon Hee Choi, Il Hee Yun, Sun Hee Suh, Dong Jun Lim, Jae Hyuung Cho, Hyuk Sang Kwon, Bong Yun Cha, Ho Young Son, Chung Gyu Park, Kun Ho Yoon
- Korean Diabetes J. 2007;31(3):208-219. Published online May 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.3.208
- 2,030 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
S: L-type voltage-dependent calcium channel (LTCC) plays a crucial role in insulin secretion from pancreatic beta cells through Ca2+ influx. In the recent report, LTCC Ca(v)1.3 subtype homozygous knock out mice showed impairment of postnatal pancreatic beta cell development as well as insulin secretion. METHODS: We performed 90% partial pancreatectomy in heterozygous Ca(v)1.3 knock out mice to investigate the effect of partial deficiency of Ca(v)1.3 gene on beta cell regeneration in the adult. Glucose homeostasis, metabolic profiles including serum insulin and lipid levels and morphologic changes of pancreatic islets were studied. RESULTS: 90% Partial pancreatectomy induced glucose intolerance only in the heterozygous knock out mice at 8 weeks after surgery. Distribution of islet size was significantly different between two groups after partial pancreatectomy; median value of islet size of heterozygote was larger than that of wild type (642.8 micrometer2 vs 1459.8 micrometer2, P < 0.01). The frequency of single beta cell unit, considered as a unit of beta cell neogenesis, was much lower in heterozygote than that of wild type (41% vs 23.3%, P < 0.05). CONCLUSION: These data suggest that Ca(v)1.3 gene deficiency is specifically associated with impairment of beta cell regeneration, especially neogensis and eventual glucose intolerance in the 90% partial pancreatectomized mice.
- Effects of Islet Transplantation on Endogenous beta-cell Regeneration after Partial Pancreatectomy in Rodents.
- Hye Seung Jung, You Ran Ahn, Seung Hoon Oh, Jung Hwa Jung, Tae Hyun Kim, You Cheol Hwang, Mira Kang, Yongsuk Bae, Young seok Kim, Jae Hoon Chung, Yong Ki Min, Myung Shik Lee, Moon Kyu Lee, Kwang Won Kim
- Korean Diabetes J. 2007;31(2):113-122. Published online March 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.2.113
- 2,250 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Islet transplantation is one of regimens supplying the deficient insulin in diabetes patients, but the effects of islet grafts on the changes of endogenous beta-cells are not clear. In the present study, we examined the changes of endogenous beta-cell mass after islet transplantation in partially pancreatectomized mice. METHODS: Balb/c mice were 70% pancreatectomized, transplanted with syngeneic islets (group IV), and were compared with pancreatectomized mice treated with insulin (group III) or no insulin (group II). Blood glucose levels and body weight were monitored. Remnant pancreas was obtained at 6 or 10 days after pancreatectomy, and immunohistochemical staining was done for the evaluation of beta-cell mass changes. RESULTS: Hyperglycemia and weight loss were induced after pancreatectomy. After islet transplantation or insulin treatment, blood glucose levels recovered to normal, and body weight started to increase. Plasma insulin levels were higher and beta-cell mass was larger in group IV than in group II (P < 0.05). Especially, the difference of beta-cell mass between them was more evident at 7 days as compared to at 3 day after transplantation. When compared to group III, group IV showed larger individual beta-cell area after 7 days and larger beta-cell mass after 3 days of islet transplantation (P < 0.05). CONCLUSION: These observations indicate that islet transplantation plays a role in enhancing remnant beta-cell regeneration after partial pancreatectomy in rodents.
- Effect of Pancreatic Islet Autotransplantation after Pacreatectomy in Patients with Benign Pancreatic Tumor.
- Jae Hwan Jee, Byung Wan Lee, Seung Hoon Oh, Ji Youn Kim, Hyun Jin Kim, Jung Hyun Noh, Sung Ho Choi, Jae Hoon Chung, Yong Ki Min, Myung Sik Lee, Moon Kyu Lee, Kwang Won Kim
- Korean Diabetes J. 2004;28(2):88-100. Published online April 1, 2004
- 1,661 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Previously, in patients suffering from insulin deficient DM after a partial or total pancreatectomy as treatment for a benign pancreatic tumor, insulin treatment has only led to severe fluctuation in the blood glucose level, and frequently to sudden hypoglycemia due to glucagon deficiency and lack of delicate insulin control. Several worldwide reports have suggested that autologous transplantation of islet cells isolated from an unaffected portion of a resected pancreas, mostly for the cure of chronic pancreatitis or a pancreatic tumor without immunosuppressive agent treatment, resulted in good glycemic control, and even in the prevention of DM. Attempts were made to evaluate the effect of islet autotrans-plantation for glycemic control in eight patients undergoing a pancreatectomy for a benign pancreatic tumor. METHOD: Between December 2001 and October 2003, an islet autotransplantation was performed in eight patients patholologically confirmed with benign pancreatic tumors following a pancreatectomy. There was no past medical history of DM in any of the patients, but impaired glucose tolerance(IGT) was detected in 2 patients on a 75g oral glucose tolerance test(oral GTT), and was also suspected in a pre-pancreatectomy state patient. Islets were isolated by ductal perfusion, using the cold collagenase P and semi-automated method, and purified on a density gradients using a COBE 2991 cell processor or tube system of Ficoll solution. After being confirmed as a benign pancreatic tumor, the cultured islet cells were transplanted to the liver through the portal vein. Each patient was transplanted with a mean islet mass of 3,190+/-896 islet equivalents per kilogram of body weight. The median follow-up period was 12 months, with the longest being 36 months. All patients underwent follow-up for oral GTT, HbA1c and complication of DM, pancreatectomy, or transplantation within this period. RESULTS: On the 75g oral GTT, a normal glucose tolerance(NGT) was maintained until the last follow-up month in five of the eight patients undergoing islet autotransplantation. DM recurred in three of the eight patients undergoing islet autotransplantation, with to cases in a state of IGT and 1 case of NGT at the initial stage. The HbA1c levels were not significantly changed between pre-pancreatectomy and post-islet transplantation period. The amplitude of the decrease in the postprandial 2 hour glucose level was larger than that of the fasting glucose level between the pre- and post-transplantation periods, but this was not statistically. Also, the elevation of the postprandial C-peptide level was larger than the fasting C-peptide during the post-transplantation period, but again, this was not significant. No complications occurred in relation with the islet transplantation, portography, DM and hypoglycemia. CONCLUSION: Islet transplantation could prevent and reverse the diabetic process in patients undergoing a pancreatectomy for a benign pancreatic tumor, with some exception such as those with a small transplanted islet mass or with initial insulin resistance. The 2 hour postprandial changes in the glucose and C- peptide levels on the oral GTT somewhat reflected insulin secretory function of the remaining and newly transplanted islet cells. Pancreatic islet autotransplantation is the most prospective method for the prevention or cure of insulin deficient DM following a pancreatectomy for a benign pancreatic tumor.
- The Changes of Beta Cell Mass and Islet Morphology in OLETF (Otsuka Long Evans Tokushima Fatty) Rats After Partial Pancreatectomy .
- Seung Hyun Ko, Kun Ho Yoon, Sun Hee Suh, Yu Bae Ahn, Soon Jib Yoo, Ki Ho Song, Hyun Shik Son, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2001;25(1):50-62. Published online February 1, 2001
- 964 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Insulin resistance and incomplete beta cell compensation play a major role for development of type 2 diabetes. When insulin resistance were induced by any cause, appropriate beta-cell proliferation is a key factor for maintaining the normal glucose metabolism. Compensatory beta-cell proliferation for adapting to increased insulin resistance might be achieved by neogenesis of beta-cell from duct cells, replication of preexisting beta-cells and also inhibition of beta-cell apoptosis. Previously incomplete beta-cell compensation was observed in OLETF rat, animal model of type 2 diabetes, after partial pancreatectomy, but there were no reports about the underlying pathogenesis. Therefore, this study was designed to study on the mechanism of incomplete beta-cell compensation in OLETF rat after partial pancreatectomy especially focus on beta-cell proliferation. METHODS: 12 week-old OLETF (Otsuka Long Evans Tokushima Fatty) rats weighing 280-320 g were used. 80% partial pancreatectomy was done. Experimental animals were divided into the 4 subgroups by date of killing after surgery: 0, 3, 90 days. After glucose tolerance test, pancreas remnant was excised and immunohistochemical staining was done for insulin to quantify the beta cell mass by point-counting method and also observed the amount of fibrosis of the islets after Masson's trichrome staining of the pancreas. RESULTS: We observed that impaired glucose tolerance or diabetes were developed after 80% pancreatectomy. We observed rapidly proliferating duct cells in the adjacent area of common pancreatic duct and main duct even up to 90 days after partial pancreatectomy. In OLETF rats, beta cell mass was not increased enough compared to LETO rats and some destructive features of islet architectures were noted at 90 days after pancreatectomy. CONCLUSION: The changes of beta cell mass seems to be a dynamic process adjusting to metabolic demand. Severe hyperglycemia and islet disorganization were apparent in OLETF rats despite of existence of beta cell regeneration and renewal process. So it seemed that hyperglycemia accelerated aging process or senescence of beta cells in OLETF rats.
- The Changes of Expression of Intermediate Flament in Pancreatic Duct Cells During Proliferation and Differentiation after 90% Pancreatectomy in Rats.
- Seung Hyeon Ko, Kun Ho Yoon, Sun Hee Seo, Jung Min Lee, Ki Won Oh, Sang Ah Chang, Hye Soo Kim, Yoo Bae Ahn, Hyun Shik Son, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2000;24(2):191-201. Published online January 1, 2001
- 1,055 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Neogenesis of the beta calls from ductal cells is the main mechanism of the increased beta cell mass after partial pancreatectomy. For the transdifferentiation from the duct cells to the beta cells, de-differentiation of the duct cells is needed because duct cells are also terminally differentiated cells already. But there was no clear evidence of de-differentiation of the duct cells during duct call proliferation so far. Herein we report the changes of intermediate filament protein expression in rapidly proliferating duct cells after partial pancreatectomy for the evidence of de-differentiation of the duct cells. METHODS: 45 week-old Sprague-Dawley rats weighing 80~120 g were used. 90% partial pancreatectomy was done. Experimental animals were divided into 5 subgroups by date of killing after surgery: 1, 3, 7, 14, 30 days, Pancreas remnant was excised and immunohistochemical stain was done for pancytokeratin (Pan-CK) as a epithelial cell marker and vimentin (VT) as a mesenchymal cell marker. We observed the double stained slide with pan-CK and VT antibody using confocal microscope for costaining analysis over time. The sections were also immunostained with anti-insulin antibody for the quantification of the beta cell mass by point-counting methods. RESULTS: We observed impaired glucose tolerance and diabetes were developed affer 90% pancreatectomy. Significant increase of the weight of pancreatic remnant, beta cell and duct cell mass were observed about 14 days after pancreatectomy. We observed the co-expression of VT and pan-CK intermediate filament protein in rapidly proliferating duct cells in the area of common pancreatic duct and main duct at one day after partial pancreatectomy. 3 days affer partial pancreatectomy, VT and pan-CK costained duct cells were mainly observed in the rageneration focus of the duct cell proliferation. 30 days after partial pancreatectomy, we could not find any costaining duct calls in the remnant pancreas. CONCLUSION: The vimentin intermediate filament, a marker of mesenchymal cell was expressed in proliferating ductal cells after pancreatectomy. We could suspect that pancytokeratin and vimentin co-expression is a good marker for de-differentiation of proliferating duct cells.

 KDA
KDA First
First Prev
Prev





