
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
- Pharmacological and Nonpharmacological Treatments for Painful Diabetic Peripheral Neuropathy
- Han Na Jang, Tae Jung Oh
- Diabetes Metab J. 2023;47(6):743-756. Published online September 6, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0018
- 4,146 View
- 559 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
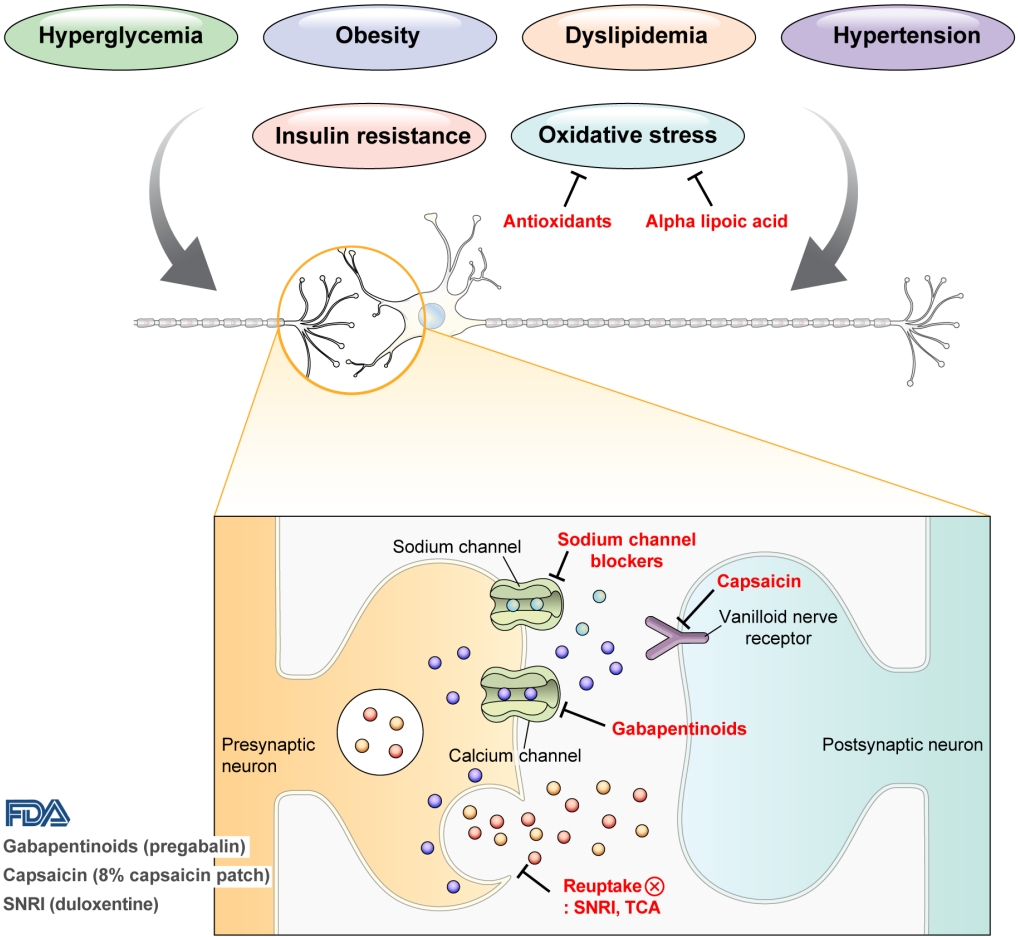
ePub - Diabetic peripheral neuropathy (DPN) is one of the most prevalent chronic complications of diabetes. The lifetime prevalence of DPN is thought to be >50%, and 15%–25% of patients with diabetes experience neuropathic pain, referred to as “painful DPN.” Appropriate treatment of painful DPN is important because this pain contributes to a poor quality of life by causing sleep disturbance, anxiety, and depression. The basic principle for the management of painful DPN is to control hyperglycemia and other modifiable risk factors, but these may be insufficient for preventing or improving DPN. Because there is no promising diseasemodifying medication for DPN, the pain itself needs to be managed when treating painful DPN. Drugs for neuropathic pain, such as gabapentinoids, serotonin–norepinephrine reuptake inhibitors, tricyclic antidepressants, alpha-lipoic acid, sodium channel blockers, and topical capsaicin, are used for the management of painful DPN. The U.S. Food and Drug Administration (FDA) has approved pregabalin, duloxetine, tapentadol, and the 8% capsaicin patch as drugs for the treatment of painful DPN. Recently, spinal cord stimulation using electrical stimulation is approved by the FDA for the treatment for painful DPN. This review describes the currently available pharmacological and nonpharmacological treatments for painful DPN.
-
Citations
Citations to this article as recorded by- J-2156, a small molecule somatostatin type 4 receptor agonist, alleviated hindpaw hypersensitivity in the streptozotocin-induced rat model of painful diabetic neuropathy but with a 2-fold decrease in potency at an advanced stage in the model, mimicking mo
A. Kuo, M. Z. Imam, R. Li, L. Lin, A. Raboczyj, A. E. Bohmer, J. R. Nicholson, L. Corradini, M. T. Smith
Frontiers in Pharmacology.2024;[Epub] CrossRef - The Chronic Wound–Related Pain Model
Kevin Woo
Clinics in Geriatric Medicine.2024;[Epub] CrossRef
- J-2156, a small molecule somatostatin type 4 receptor agonist, alleviated hindpaw hypersensitivity in the streptozotocin-induced rat model of painful diabetic neuropathy but with a 2-fold decrease in potency at an advanced stage in the model, mimicking mo
- Technology/Device
- Comparison of Laser and Conventional Lancing Devices for Blood Glucose Measurement Conformance and Patient Satisfaction in Diabetes Mellitus
- Jung A Kim, Min Jeong Park, Eyun Song, Eun Roh, So Young Park, Da Young Lee, Jaeyoung Kim, Ji Hee Yu, Ji A Seo, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):936-940. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0293
- 5,340 View
- 256 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Self-monitoring of capillary blood glucose is important for controlling diabetes. Recently, a laser lancing device (LMT-1000) that can collect capillary blood without skin puncture was developed. We enrolled 150 patients with type 1 or 2 diabetes mellitus. Blood sampling was performed on the same finger on each hand using the LMT-1000 or a conventional lancet. The primary outcome was correlation between glucose values using the LMT-1000 and that using a lancet. And we compared the pain and satisfaction of the procedures. The capillary blood sampling success rates with the LMT-1000 and lancet were 99.3% and 100%, respectively. There was a positive correlation (r=0.974, P<0.001) between mean blood glucose levels in the LMT-1000 (175.8±63.0 mg/dL) and conventional lancet samples (172.5±63.6 mg/dL). LMT-1000 reduced puncture pain by 75.0% and increased satisfaction by 80.0% compared to a lancet. We demonstrated considerable consistency in blood glucose measurements between samples from the LMT-1000 and a lancet, but improved satisfaction and clinically significant pain reduction were observed with the LMT-1000 compared to those with a lancet.
-
Citations
Citations to this article as recorded by- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Chul Kyu Yun, Eui Kyung Choi, Hyung Jin Kim, Jaeyoung Kim, Byung Cheol Park, Kyuhee Park, Byung Min Choi
Journal of Perinatology.2024;[Epub] CrossRef
- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
- Others
- Increased Nociceptive Responses in Streptozotocin-Induced Diabetic Rats and the Related Expression of Spinal NR2B Subunit of
N -Methyl-D-Aspartate Receptors - Che Aishah Nazariah Ismail, Rapeah Suppian, Che Badariah Abd Aziz, Khalilah Haris, Idris Long
- Diabetes Metab J. 2019;43(2):222-235. Published online November 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0020
- 4,768 View
- 52 Download
- 12 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study investigated the role of NR2B in a modulated pain process in the painful diabetic neuropathy (PDN) rat using various pain stimuli.
Methods Thirty-two Sprague-Dawley male rats were randomly allocated into four groups (n=8): control, diabetes mellitus (DM) rats and diabetic rats treated with ifenprodil at a lower dose (0.5 µg/day) (I 0.5) or higher dose (1.0 µg/day) (I 1.0). DM was induced by a single injection of streptozotocin at 60 mg/kg on day 0 of experimentation. Diabetic status was assessed on day 3 of the experimentation. The responses on both tactile and thermal stimuli were assessed on day 0 (baseline), day 14 (pre-intervention), and day 22 (post-intervention). Ifenprodil was given intrathecally for 7 days from day 15 until day 21. On day 23, 5% formalin was injected into the rats' hind paw and the nociceptive responses were recorded for 1 hour. The rats were sacrificed 72 hours post-formalin injection and an analysis of the spinal NR2B expression was performed.
Results DM rats showed a significant reduction in pain threshold in response to the tactile and thermal stimuli and higher nociceptive response during the formalin test accompanied by the higher expression of phosphorylated spinal NR2B in both sides of the spinal cord. Ifenprodil treatment for both doses showed anti-allodynic and anti-nociceptive effects with lower expression of phosphorylated and total spinal NR2B.
Conclusion We suggest that the pain process in the streptozotocin-induced diabetic rat that has been modulated is associated with the higher phosphorylation of the spinal NR2B expression in the development of PDN, which is similar to other models of neuropathic rats.
-
Citations
Citations to this article as recorded by- Painful diabetic neuropathy: The role of ion channels
Qi Wang, Yifei Ye, Linghui Yang, Lifan Xiao, Jin Liu, Wensheng Zhang, Guizhi Du
Biomedicine & Pharmacotherapy.2024; 173: 116417. CrossRef - Therapeutic potential of progesterone in spinal cord injury‐induced neuropathic pain: At the crossroads between neuroinflammation and N‐methyl‐D‐aspartate receptor
Sol Ferreyra, Susana González
Journal of Neuroendocrinology.2023;[Epub] CrossRef - Chemical, pharmacodynamic and pharmacokinetic characterization of the GluN2B receptor antagonist 3-(4-phenylbutyl)-2,3,4,5-tetrahydro-1H-3-benzazepine-1,7-diol – starting point for PET tracer development
Marvin Korff, Ruben Steigerwald, Elena Bechthold, Dirk Schepmann, Julian A. Schreiber, Sven G. Meuth, Guiscard Seebohm, Bernhard Wünsch
Biological Chemistry.2023; 404(4): 279. CrossRef - Mechanisms of Transmission and Processing of Pain: A Narrative Review
Girolamo Di Maio, Ines Villano, Ciro Rosario Ilardi, Antonietta Messina, Vincenzo Monda, Ashlei Clara Iodice, Chiara Porro, Maria Antonietta Panaro, Sergio Chieffi, Giovanni Messina, Marcellino Monda, Marco La Marra
International Journal of Environmental Research and Public Health.2023; 20(4): 3064. CrossRef - Indazole as a Phenol Bioisostere: Structure–Affinity Relationships of GluN2B-Selective NMDA Receptor Antagonists
Judith Lüken, Gunnar Goerges, Nadine Ritter, Paul Disse, Julian A. Schreiber, Judith Schmidt, Bastian Frehland, Dirk Schepmann, Guiscard Seebohm, Bernhard Wünsch
Journal of Medicinal Chemistry.2023; 66(16): 11573. CrossRef - Synthesis of oxazolo‐annulated 3‐benzazepines designed by merging two negative allosteric NMDA receptor modulators
Alexander Markus, Dirk Schepmann, Bernhard Wünsch
Archiv der Pharmazie.2022;[Epub] CrossRef - Phenol—Benzoxazolone bioisosteres: Synthesis and biological evaluation of tricyclic GluN2B‐selective N‐methyl‐d‐aspartate receptor antagonists
Alexander Markus, Julian A. Schreiber, Gunnar Goerges, Bastian Frehland, Guiscard Seebohm, Dirk Schepmann, Bernhard Wünsch
Archiv der Pharmazie.2022;[Epub] CrossRef - Ifenprodil Reduced Expression of Activated Microglia, BDNF and DREAM Proteins in the Spinal Cord Following Formalin Injection During the Early Stage of Painful Diabetic Neuropathy in Rats
Che Aishah Nazariah Ismail, Rapeah Suppian, Che Badariah Ab Aziz, Idris Long
Journal of Molecular Neuroscience.2021; 71(2): 379. CrossRef - Ifenprodil Stereoisomers: Synthesis, Absolute Configuration, and Correlation with Biological Activity
Elena Bechthold, Julian A. Schreiber, Kirstin Lehmkuhl, Bastian Frehland, Dirk Schepmann, Freddy A. Bernal, Constantin Daniliuc, Inés Álvarez, Cristina Val Garcia, Thomas J. Schmidt, Guiscard Seebohm, Bernhard Wünsch
Journal of Medicinal Chemistry.2021; 64(2): 1170. CrossRef - The anti-diabetic effects of betanin in streptozotocin-induced diabetic rats through modulating AMPK/SIRT1/NF-κB signaling pathway
Nasim Abedimanesh, Somayyeh Asghari, Kosar Mohammadnejad, Zahra Daneshvar, Soudeh Rahmani, Samaneh Shokoohi, Amir Hasan Farzaneh, Seyed Hojjat Hosseini, Iraj Jafari Anarkooli, Maryam Noubarani, Sina Andalib, Mohammad Reza Eskandari, Behrooz Motlagh
Nutrition & Metabolism.2021;[Epub] CrossRef - Diabetic neuropathy and neuropathic pain: a (con)fusion of pathogenic mechanisms?
Nigel A. Calcutt
Pain.2020; 161(Supplement): S65. CrossRef - N-Acetylcysteine causes analgesia in a mouse model of painful diabetic neuropathy
Serena Notartomaso, Pamela Scarselli, Giada Mascio, Francesca Liberatore, Emanuela Mazzon, Santa Mammana, Agnese Gugliandolo, Giorgio Cruccu, Valeria Bruno, Ferdinando Nicoletti, Giuseppe Battaglia
Molecular Pain.2020; 16: 174480692090429. CrossRef - Effect of aerobic exercise on innate immune responses and inflammatory mediators in the spinal cord of diabetic rats
A. Kaki, M. Nikbakht, A.H. Habibi, H.F. Moghadam
Comparative Exercise Physiology.2020; 16(4): 293. CrossRef
- Painful diabetic neuropathy: The role of ion channels
- Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus in Korea
- Seung-Hyun Ko, Bong-Yun Cha
- Diabetes Metab J. 2012;36(1):6-12. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.6
- 4,592 View
- 83 Download
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetic peripheral neuropathy (DPN), a common and troublesome complication in patients with type 2 diabetes mellitus (T2DM), contributes to a higher risk of diabetic foot ulcer and lower limb amputation. These situations can negatively impact the quality of life of affected individuals. Despite its high prevalence and clinical importance, most diabetes mellitus patients not only do not recognize the presence of diabetic neuropathy, but also do not report their symptoms to physicians or other health care providers. Therefore, DPN is usually under diagnosed and undertreated. For early detection and appropriate intervention for DPN, a careful history, physical with neurologic examination, and prompt treatment are needed in T2DM patients.
-
Citations
Citations to this article as recorded by- Pramipexole protects against diabetic neuropathy: Effect on oxidative stress, TLR4/IRAK-1/TRAF-6/NF-κB and downstream inflammatory mediators
Nada H. Eisa, Sahar A Helmy, Dalia H. El-Kashef, Mohamed El-Sherbiny, Nehal M. Elsherbiny
International Immunopharmacology.2024; 128: 111514. CrossRef - Diabetic peripheral neuropathy among adult type 2 diabetes patients in Adama, Ethiopia: health facility-based study
Yohannes Mekuria Negussie, Nardos Tilahun Bekele
Scientific Reports.2024;[Epub] CrossRef - Phenotypical characterization of exteroceptive sensation and pain symptoms on diabetic patients
Inaeh de Paula Oliveira, Victória Regina da Silva Oliveira, Heloísa Alonso‐Matielo, Beatriz Magalhães Eng, Daniel Ciampi de Andrade, Manoel Jacobsen Teixeira, Milena Cristina Dias Calsaverini, Fernando de Quadros Ribeiro, José Deney Alves Araújo, Helder T
Pain Practice.2024;[Epub] CrossRef - New Horizons in Diabetic Neuropathies: An Updated Review on their
Pathology, Diagnosis, Mechanism, Screening Techniques, Pharmacological,
and Future Approaches
Namra Aziz, Biswajit Dash, Pranay Wal, Prachi Kumari, Poonam Joshi, Ankita wal
Current Diabetes Reviews.2024;[Epub] CrossRef - Time to diabetic neuropathy and its predictors among adult type 2 diabetes mellitus patients in Amhara regional state Comprehensive Specialized Hospitals, Northwest Ethiopia, 2022: A retrospective follow up study
Sharie Tantigegn, Atsede Alle Ewunetie, Moges Agazhe, Abiot Aschale, Muluye Gebrie, Gedefaw Diress, Bekalu Endalew Alamneh, James Nyirenda
PLOS ONE.2023; 18(4): e0284568. CrossRef - Nutraceuticals: A Promising Approach Towards Diabetic Neuropathy
Sakshi Bajaj, Sumeet Gupta
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(5): 581. CrossRef - Role of oxidative stress in diabetes-induced complications and their management with antioxidants
Hasandeep Singh, Rajanpreet Singh, Arshdeep Singh, Harshbir Singh, Gurpreet Singh, Sarabjit Kaur, Balbir Singh
Archives of Physiology and Biochemistry.2023; : 1. CrossRef - Diabetic Peripheral Neuropathy Associated with Cardiovascular Risk Factors and Glucagon-Like Peptide-1 Concentrations Among Newly Diagnosed Patients with Type 2 Diabetes Mellitus
Tuan Dinh Le, Nga Phi Thi Nguyen, Thi Thanh Hoa Tran, Thuc Luong Cong, Lan Ho Thi Nguyen, Binh Do Nhu, Son Tien Nguyen, Manh Van Ngo, Trung Hoa Dinh, Hien Thi Nguyen, Kien Trung Nguyen, Cuong Duc Le
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 35. CrossRef - The relation between serum uric acid levels and diabetic peripheral neuropathy in type 2 diabetes in Guilan, north of Iran
Haniye Sadat Fayazi, Maryam Yaseri, Seyyede Sahere Mortazavi, Zahra Sharifhassan, Ali-Sina Assadinia
BMC Endocrine Disorders.2022;[Epub] CrossRef - A comparative evaluation of cardiac and neurological safety status of two commonly used oral hypoglycaemic agents in T2-DM Swiss albino mice model
Md. Ohidur Rahman, Shaheen Ahmed, Tanoy Mazumder, Md. Abdus Salam, Prodip Kumar Baral, Md. Faruk Rana, Shuvo Mitra, Sayem Hossain, Rubiya Rahman, Md. Saddam Hussain
Metabolism Open.2022; 14: 100191. CrossRef - Increased expression of BDNF and inflammatory biomarkers in type 2 diabetes-related claustrophobia: A case report
Ankita Srivastava, BashairM Mussa, Salahedeen Abusnana
Advances in Biomedical and Health Sciences.2022; 1(3): 175. CrossRef - Drug repurposing – A search for novel therapy for the treatment of diabetic neuropathy
Arpita Paul, Mohit Kumar, Parikshit Das, Nilayan Guha, Mithun Rudrapal, Md. Kamaruz Zaman
Biomedicine & Pharmacotherapy.2022; 156: 113846. CrossRef - Comparison of Neutrophyl Lymphocyte Ratio and Nerve Conduction Study Between Male Type 2 Diabetes Mellitus With or Without Peripheral Neuropathy Complication
Martha Kurnia Kusumawardani, Surdiana, I Putu Alit Pawana, Sony Wibisono
Indonesian Journal of Physical Medicine and Rehabilitation.2022; 11(01): 33. CrossRef - Is health related quality of life influenced by diabetic neuropathic pain among type II diabetes mellitus patients in Ethiopia?
Hiwot Degu, Abigiya Wondimagegnehu, Yared Mamushet Yifru, Ayele Belachew, Rayaz A. Malik
PLOS ONE.2019; 14(2): e0211449. CrossRef - Improving vibration perception in a patient with type 2 diabetes and sensory peripheral neuropathy
Liezel Ennion, Juha Hijmans
South African Journal of Physiotherapy.2019;[Epub] CrossRef - Fas-mediated apoptosis and peripheral polyneuropathy in type 2 diabetes mellitus
Mowaffak M. Abd Elhameed, Noha A. Elsawy, Magdy H. Zekry Mgalaa, Sarah S. El-Tawab, Reham A. Abo Elwafa, Marwa R. Abd Elfadeel
Egyptian Rheumatology and Rehabilitation.2019; 46(4): 321. CrossRef - The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice
Jung Hwan Park, Dong Sun Kim
Diabetes & Metabolism Journal.2018; 42(5): 442. CrossRef - Transplantation of human mobilized mononuclear cells improved diabetic neuropathy
Se Hee Min, Jung Hee Kim, Yu Mi Kang, Seung Hak Lee, Byung-Mo Oh, Kyou-Sup Han, Meihua Zhang, Hoe Suk Kim, Woo Kyung Moon, Hakmo Lee, Kyong Soo Park, Hye Seung Jung
Journal of Endocrinology.2018; 239(3): 277. CrossRef - Do we underestimate influences of diabetic mononeuropathy or polyneuropathy on hand functional performance and life quality?
Chien‐Ju Yang, Hsiu‐Yun Hsu, Chieh‐Hsiang Lu, Yen‐Li Chao, Haw‐Yen Chiu, Li‐Chieh Kuo
Journal of Diabetes Investigation.2018; 9(1): 179. CrossRef - Response: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (Diabetes Metab J 2018;42:442–6)
Jung Hwan Park, Dong Sun Kim
Diabetes & Metabolism Journal.2018; 42(6): 546. CrossRef - Molecular mechanism of diabetic neuropathy and its pharmacotherapeutic targets
Saikat Dewanjee, Sonjit Das, Anup Kumar Das, Niloy Bhattacharjee, Anjum Dihingia, Tarun K. Dua, Jatin Kalita, Prasenjit Manna
European Journal of Pharmacology.2018; 833: 472. CrossRef - ANTIOXIDANT STATUS IN DIABETIC NEUROPATHY
Giriraja Vrushabaiah Kanakapura, Pavitra Chandrashekar Bangalore, Bindumathi Pula Lakshmi
Journal of Evidence Based Medicine and Healthcare.2017; 4(78): 4588. CrossRef - Association of diabetic vascular complications with poor sleep complaints
Ling-Ling Meng, Ying Liu, Rui-Na Geng, Yun-Zhao Tang, Dai-Qing Li
Diabetology & Metabolic Syndrome.2016;[Epub] CrossRef - Response: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (Diabetes Metab J 2015;39:498-506)
Jae-Seung Yun, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(1): 85. CrossRef - Antioxidant Strategies in the Management of Diabetic Neuropathy
Ayodeji Babatunde Oyenihi, Ademola Olabode Ayeleso, Emmanuel Mukwevho, Bubuya Masola
BioMed Research International.2015; 2015: 1. CrossRef - Association of depression and sleep quality with complications of type 2 diabetes in geriatric patients
Zeynel Abidin Öztürk, Yusuf Yesil, Mehmet Emin Kuyumcu, Esen Savas, Özhan Uygun, Zeynel Abidin Sayıner, Yalçın Kepekçi
Aging Clinical and Experimental Research.2015; 27(4): 533. CrossRef - Incidence trends and associated factors of diabetes mellitus in Korean children and adolescents: a retrospective cohort study in Busan and Gyeongnam
Jung Hyun Lee, Yu-Mi Kim, Min Jung Kwak, Su Yung Kim, Hyun-Ji Kim, Chong Kun Cheon, Woo Yeong Chung, Im-Jeong Choi, Su Young Hong, Hee Won Chueh, Jae-Ho Yoo
Annals of Pediatric Endocrinology & Metabolism.2015; 20(4): 206. CrossRef - Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
Jin-Hee Jung, Jung-Hwa Lee, Jin-Won Noh, Jeong-Eun Park, Hee-Sook Kim, Joo-Wha Yoo, Bok-Rye Song, Jeong-rim Lee, Myeong-Hee Hong, Hyang-Mi Jang, Young Na, Hyun-Joo Lee, Jeong-Mi Lee, Yang-Gyo Kang, Sun-Young Kim, Kang-Hee Sim
Diabetes & Metabolism Journal.2015; 39(4): 307. CrossRef - Diabetic Peripheral Neuropathy in Ambulatory Patients with Type 2 Diabetes in a General Hospital in a Middle Income Country: A Cross-Sectional Study
María de los Angeles Lazo, Antonio Bernabé-Ortiz, Miguel E. Pinto, Ray Ticse, German Malaga, Katherine Sacksteder, J. Jaime Miranda, Robert H. Gilman, Leighton R. James
PLoS ONE.2014; 9(5): e95403. CrossRef - Monochromatic Infrared Photo Energy in Diabetic Peripheral Neuropathy
Tarek A. Ammar
ISRN Rehabilitation.2012; 2012: 1. CrossRef
- Pramipexole protects against diabetic neuropathy: Effect on oxidative stress, TLR4/IRAK-1/TRAF-6/NF-κB and downstream inflammatory mediators
- Association of Haplotype Combinations of Calpain-10 Gene Polymorphisms and the Metabolic Syndrome in Type 2 Diabetes.
- Eun Seok Kang, Hye Joo Kim, Sung Min Myoung, Yumie Rhee, Chul Woo Ahn, Bong Soo Cha, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Moonsuk Nam
- Korean Diabetes J. 2005;29(5):451-459. Published online September 1, 2005
- 1,296 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - OBJECTIVE: Patients with metabolic syndrome are at increased risk of developing cardiovascular disease. The combinations of the haplotype created by the alleles of three single nucleotide polymorphisms (SNPs): SNP-43, SNP-19, and SNP-63 of the Calpain 10 gene (CAPN10), have been reported to be associated with the risk of type 2 diabetes (T2DM) in many populations. The aim of this study was to examine the association of the CAPN10 polymorphisms with metabolic syndrome in Korean patients with T2DM. METHODS: Overall, 382 T2DM patients were enrolled in this study. All the subjects were genotyped according to CAPN10 SNP-43, SNP-19 and SNP-63. The restriction fragment length polymorphism method was used for the three SNPs. The baseline presence of the components of metabolic syndrome was determined. RESULTS: 265 (69.4 %) patients were found to have metabolic syndrome. Patients with the 111/121 haplotype combination showed a higher risk of hypertension than the other haplotype combinations (OR=2.334, P=0.010) and also had a significantly higher risk of having metabolic syndrome (OR=1.927, P=0.042). CONCLUSION: The results of this study suggest a role of the novel 111/121 haplotype combination created by the CAPN10 SNPs -43, -19 and -63 in the susceptibility to metabolic syndrome of T2DM patients.
- Analgesic Effects of DA-5018, a New Capsaicin Derivative, in Hyperalgesia of Experimental Diabetic Neuropathy.
- Eun Ju Bae, Soon How Kim, Moon Ho Son, Hee Kee Kim, Myeong Soo Shin, Hyun Ji Kim, Won Bae Kim
- Korean Diabetes J. 1997;21(1):91-101. Published online January 1, 2001
- 1,056 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Painful peripheral neuropathy is one of the most common complications of diabetes and not responsive to conventional analgesics. Capsaicin cream has been used to treat the pain associated with diabetic neuropathy, rheumatoid arthritis, osteoarthritis and postherpetic neuralgia. But its common side effect, burning sensation, limits the use of it. DA-5018 is a newly synthesized capsaicin derivative which shows more potent systemic and topical analgesia than capsaicin in various animal models of acute and chronic pain, but has little skin irritaion. This study was designed to evaluate the effect of DA-5018 administered systemically or topically on hyperalgesia in streptozotocin-induced diabetic and galactosaemic rats. METHODS: One group of SD rats was treated with streptozotocin(60mg/kg, I.v.) and the pain thresholds were determined weekly by Randall-Selitto paw pressure test. And the other group of SD rats was maintained on 50%-galactose diet until 4~5 weeks and the pain thresholds were determined as well, Drugs were administered subcutaneously once a day for 7 days or topically to the paw for 5 hours a day for 10 days at a time when the hyperalgesia was already present. The increase of pain thresholds by drug was regarded as an indication of analgesia. RESULTS: Streptozotocin-diabetic rats displayed a reduction of pain threshold. Similarly, galactosefeeding resulted in significant reduction of pain threshold. It is concluded that hyperalgesia is a constant feature of sensory dysfunction in experimental models of diabetic and nutritional neuropathy. DA-5018(0.2, 0.5mg/kg, s.c.) produced significant antinociception with efficacy similar to that of capsaicin(10mg/kg, s.c.) in streptozotocin-induced hyperalgesia and furthermore, no tolerance developed for 7 days. And this analgesic effect was superior to desipramine(10mg/kg, s.c.). But ketoprofen(10mg/kg, s.c.) produced no analgesia. Topically, 0.3% DA-5018 cream was as effective as Zostrix-HP(capsaicin 0.075%) both in streptozotocin-diabetic and galactosefed rats while Kenofen gel(ketoprofen 3%) was ineffective to reduce pain. CONCLUSION: These results demonstrate the potent analgesic efficacy of DA-5018 in diabetic pain models and suggest that topical DA-5018 cream may relieves pain caused by diabetic neuropathy offering an alternative for patients not responsive to other treatments or unable to tolerate capsaicin.

 KDA
KDA
 First
First Prev
Prev





