
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Diabetes Promotes Myocardial Fibrosis via AMPK/EZH2/PPAR-γ Signaling Pathway
- Shan-Shan Li, Lu Pan, Zhen-Ye Zhang, Meng-Dan Zhou, Xu-Fei Chen, Ling-Ling Qian, Min Dai, Juan Lu, Zhi-Ming Yu, Shipeng Dang, Ru-Xing Wang
- Received February 3, 2023 Accepted November 13, 2023 Published online February 27, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0031 [Epub ahead of print]
- 901 View
- 54 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
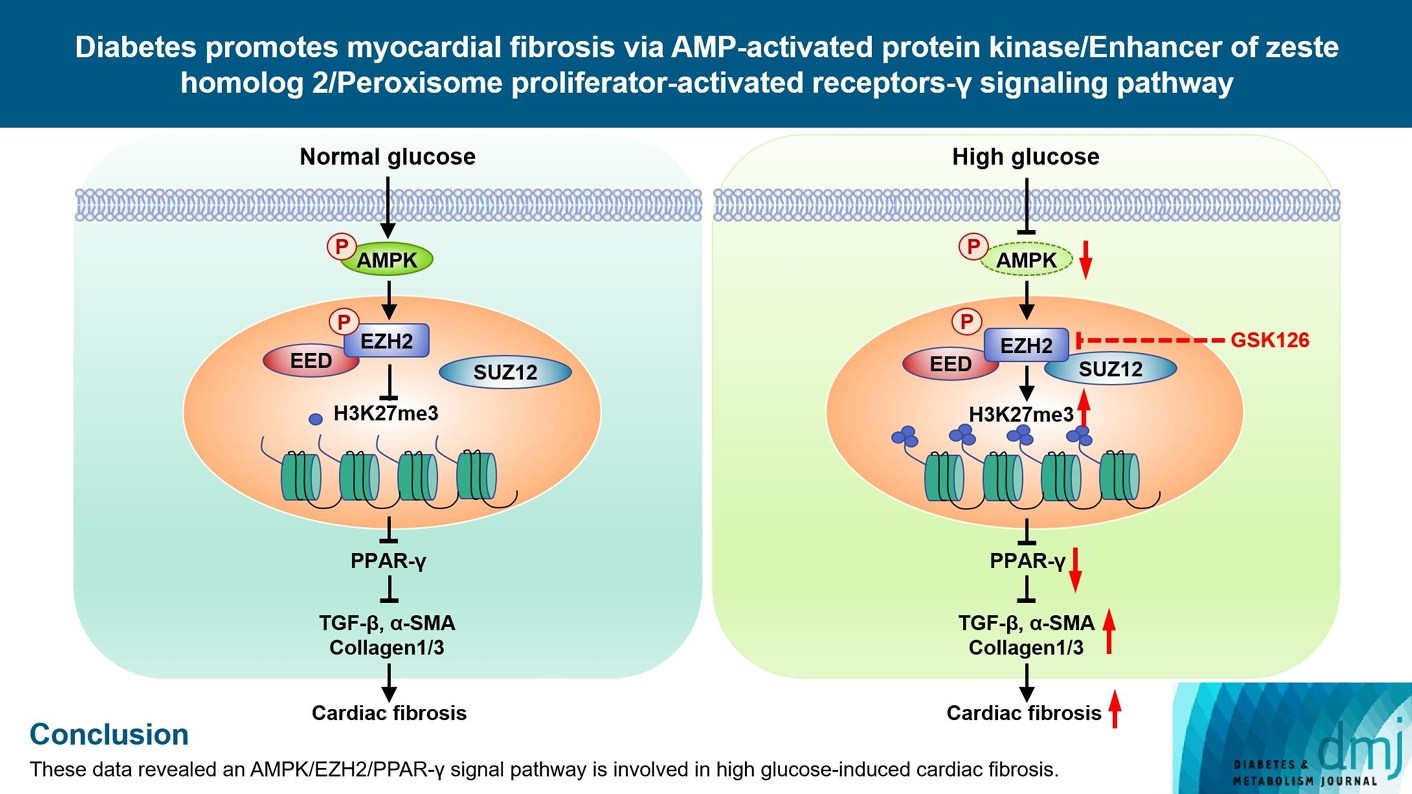
Diabetes-induced cardiac fibrosis is one of the main mechanisms of diabetic cardiomyopathy. As a common histone methyltransferase, enhancer of zeste homolog 2 (EZH2) has been implicated in fibrosis progression in multiple organs. However, the mechanism of EZH2 in diabetic myocardial fibrosis has not been clarified.
Methods
In the current study, rat and mouse diabetic model were established, the left ventricular function of rat and mouse were evaluated by echocardiography and the fibrosis of rat ventricle was evaluated by Masson staining. Primary rat ventricular fibroblasts were cultured and stimulated with high glucose (HG) in vitro. The expression of histone H3 lysine 27 (H3K27) trimethylation, EZH2, and myocardial fibrosis proteins were assayed.
Results
In STZ-induced diabetic ventricular tissues and HG-induced primary ventricular fibroblasts in vitro, H3K27 trimethylation was increased and the phosphorylation of EZH2 was reduced. Inhibition of EZH2 with GSK126 suppressed the activation, differentiation, and migration of cardiac fibroblasts as well as the overexpression of the fibrotic proteins induced by HG. Mechanical study demonstrated that HG reduced phosphorylation of EZH2 on Thr311 by inactivating AMP-activated protein kinase (AMPK), which transcriptionally inhibited peroxisome proliferator-activated receptor γ (PPAR-γ) expression to promote the fibroblasts activation and differentiation.
Conclusion
Our data revealed an AMPK/EZH2/PPAR-γ signal pathway is involved in HG-induced cardiac fibrosis.
- Adipose Gene Expression Profiles Related to Metabolic Syndrome Using Microarray Analyses in Two Different Models
- Hye Jin Yoo, Hwan-Jin Hwang, Tae Woo Jung, Ja Young Ryu, Ho Cheol Hong, Hae Yoon Choi, Sei Hyun Baik, Kyung Mook Choi
- Diabetes Metab J. 2014;38(5):356-365. Published online October 17, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.5.356
- 4,204 View
- 43 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Peroxisome proliferator-activated receptor-γ (PPAR-γ) agonist has a wide-ranging influence on multiple components of metabolic syndrome. The Otsuka Long-Evans Tokushima Fatty (OLETF) rat is a useful animal model of metabolic syndrome. To determine genes related to metabolic syndrome, we examined overlapping genes that are simultaneously decreased by PPAR-γ agonists and increased in OLETF rats using microarrays in two different models.
Methods In the first microarray analysis, PPAR-γ agonist-treated
db/db mice were compared to standard diet-feddb/db mice. In the second microarray analysis, OLETF rats were compared to Long-Evans Tokushima Otsuka (LETO) rats (control of OLETF rats).Results Among the overlapping genes, in the present study, we validated that lipocalin-2 expression was significantly decreased in the visceral adipose tissue of PPAR-γ agonist-treated
db/db mice compared to standard diet-feddb/db mice and increased in OLETF rats compared to LETO rats using real time reverse transcription polymerase chain reaction. Furthermore, we showed for the first time that lipocalin-2 expression was significantly increased in the visceral adipose tissues of obese humans compared with nonobese humans. In addition, the expression level of lipocalin-2 in human visceral adipose tissue had a significant positive correlation with body mass index, serum interleukin-6, adipocyte fatty acid binding protein levels, and white blood cell count.Conclusion Lipocalin-2 was confirmed to be a significant adipokine affected by PPAR-γ agonist and obesity in the present study. Also, for the first time in human visceral adipose tissue, it was determined that the expression of lipocalin-2 from obese humans was significantly increased and correlated with circulating inflammatory markers.
-
Citations
Citations to this article as recorded by- Lipocalin‐2—The myth of its expression and function
Dahui Li, Wai Yan Sun, Bowen Fu, Aimin Xu, Yu Wang
Basic & Clinical Pharmacology & Toxicology.2020; 127(2): 142. CrossRef - Lipocalin-2 counteracts metabolic dysregulation in obesity and diabetes
Ioanna Mosialou, Steven Shikhel, Na Luo, Peristera Ioanna Petropoulou, Konstantinos Panitsas, Brygida Bisikirska, Nyanza J. Rothman, Roxane Tenta, Bertrand Cariou, Matthieu Wargny, Elisabeth Sornay-Rendu, Thomas Nickolas, Mishaela Rubin, Cyrille B. Confav
Journal of Experimental Medicine.2020;[Epub] CrossRef - Metabolism and adult neurogenesis: Towards an understanding of the role of lipocalin-2 and iron-related oxidative stress
Ana Catarina Ferreira, Nuno Sousa, João M. Bessa, João Carlos Sousa, Fernanda Marques
Neuroscience & Biobehavioral Reviews.2018; 95: 73. CrossRef - LH-21, A Peripheral Cannabinoid Receptor 1 Antagonist, Exerts Favorable Metabolic Modulation Including Antihypertensive Effect in KKAy Mice by Regulating Inflammatory Cytokines and Adipokines on Adipose Tissue
Ziqi Dong, Hui Gong, Yadan Chen, Hong Wu, Jun Wu, Yinghong Deng, Xinmao Song
Frontiers in Endocrinology.2018;[Epub] CrossRef - Lipocalin 2 produces insulin resistance and can be upregulated by glucocorticoids in human adipose tissue
Prasad G. Kamble, Maria J. Pereira, Cherno O. Sidibeh, Sam Amini, Magnus Sundbom, Joey Lau Börjesson, Jan W. Eriksson
Molecular and Cellular Endocrinology.2016; 427: 124. CrossRef - Serum lipocalin-2 levels are positively associated with not only total body fat but also visceral fat area in Chinese men
Yuqi Luo, Xiaojing Ma, Xiaoping Pan, Yiting Xu, Qin Xiong, Yunfeng Xiao, Yuqian Bao, Weiping Jia
Medicine.2016; 95(30): e4039. CrossRef - From the periphery to the brain: Lipocalin-2, a friend or foe?
Ana C. Ferreira, Sandro Dá Mesquita, João C. Sousa, Margarida Correia-Neves, Nuno Sousa, Joana A. Palha, Fernanda Marques
Progress in Neurobiology.2015; 131: 120. CrossRef
- Lipocalin‐2—The myth of its expression and function
- Targeting the Peroxisome Proliferator-Activated Receptor-γ to Counter the Inflammatory Milieu in Obesity
- Cesar Corzo, Patrick R. Griffin
- Diabetes Metab J. 2013;37(6):395-403. Published online December 12, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.6.395
- 3,737 View
- 30 Download
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Adipose tissue, which was once viewed as a simple organ for storage of triglycerides, is now considered an important endocrine organ. Abnormal adipose tissue mass is associated with defects in endocrine and metabolic functions which are the underlying causes of the metabolic syndrome. Many adipokines, hormones secreted by adipose tissue, regulate cells from the immune system. Interestingly, most of these adipokines are proinflammatory mediators, which increase dramatically in the obese state and are believed to be involved in the pathogenesis of insulin resistance. Drugs that target peroxisome proliferator-activated receptor-γ have been shown to possess anti-inflammatory effects in animal models of diabetes. These findings, and the link between inflammation and the metabolic syndrome, will be reviewed here.
-
Citations
Citations to this article as recorded by- Lysine 222 in PPAR γ1 functions as the key site of MuRF2-mediated ubiquitination modification
Yucheng Fan, Fangjing Xu, Rui Wang, Jun He
Scientific Reports.2023;[Epub] CrossRef - Heart failure and diabetes: Clinical significance and epidemiology of this two‐way association
Terri Jerkins, Janet B. McGill, David S. H. Bell
Diabetes, Obesity and Metabolism.2023; 25(S3): 3. CrossRef - The pleiotropic peroxisome proliferator activated receptors: Regulation and therapeutics
Gargi Dixit, Arati Prabhu
Experimental and Molecular Pathology.2022; 124: 104723. CrossRef - The Effect of PPARγ rs1801282 Variant on Mortality Risk Among Asians With Chronic Kidney Disease: A Cohort Study and Meta-Analysis
Wei-Teing Chen, Chih-Chien Chiu, Dung-Jang Tsai, Pi-Shao Ko, Meng-Chang Lee, Hsiao-Ting Lin, Ying-Kai Chen, Wen Su, Yuh-Feng Lin, Sui-Lung Su
Frontiers in Genetics.2022;[Epub] CrossRef - Metabolic Spectrum of Liver Failure in Type 2 Diabetes and Obesity: From NAFLD to NASH to HCC
Hyunmi Kim, Da Som Lee, Tae Hyeon An, Hyun-Ju Park, Won Kon Kim, Kwang-Hee Bae, Kyoung-Jin Oh
International Journal of Molecular Sciences.2021; 22(9): 4495. CrossRef - Associations between obesity-related gene expression in maternal and cord blood and newborn adiposity: findings from the Araraquara Cohort study
P. Nakandakare, C. F. Nicoletti, N. Y. Noronha, C. B. Nonino, P. P. Argentato, N. N. Dejani, L. A. Luzia, M. M. Rogero, P. H. C. Rondó
International Journal of Obesity.2021; 45(9): 1958. CrossRef - PPARG Pro12Ala Polymorphism with CKD in Asians: A Meta-Analysis Combined with a Case-Control Study—A Key for Reaching Null Association
Hsiang-Cheng Chen, Wei-Teing Chen, Tzu-Ling Sung, Dung-Jang Tsai, Chin Lin, Hao Su, Yuh-Feng Lin, Hung-Yi Chiu, Sui-Lung Su
Genes.2020; 11(6): 705. CrossRef - Induction of peroxisome proliferator activated receptor γ (PPARγ) mediated gene expression and inhibition of induced nitric oxide production by Maerua subcordata (Gilg) DeWolf
Mebrahtom Gebrelibanos Hiben, Laura de Haan, Bert Spenkelink, Sebastiaan Wesseling, Jacques Vervoort, Ivonne M. C. M. Rietjens
BMC Complementary Medicine and Therapies.2020;[Epub] CrossRef - UPR modulation of host immunity by Pseudomonas aeruginosa in cystic fibrosis
Brahmchetna Bedi, Kuo-Chuan. Lin, Nicholas M. Maurice, Zhihong Yuan, Kaiser Bijli, Michael Koval, C. Michael Hart, Joanna B. Goldberg, Arlene Stecenko, Ruxana T. Sadikot
Clinical Science.2020; 134(14): 1911. CrossRef - Sepsis Immunometabolism: From Defining Sepsis to Understanding How Energy Production Affects Immune Response
Ioannis Koutroulis, Rachael Batabyal, Brittany McNamara, Matthew Ledda, Claire Hoptay, Robert J. Freishtat
Critical Care Explorations.2019; 1(11): e0061. CrossRef - Combining SGLT2 Inhibition With a Thiazolidinedione Additively Attenuate the Very Early Phase of Diabetic Nephropathy Progression in Type 2 Diabetes Mellitus
Eugene Han, Eugene Shin, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Frontiers in Endocrinology.2018;[Epub] CrossRef - Role of oral hypoglycemic drugs on inflammatory condition associated with type 2 diabetes mellitus
Shamim Shaikh Mohiuddin
Journal of Diabetes, Metabolic Disorders & Control.2018; 5(2): 78. CrossRef - Effects of lobeglitazone on insulin resistance and hepatic steatosis in high-fat diet-fed mice
Bong-Hoi Choi, Zhen Jin, Chin-ok Yi, Juhong Oh, Eun Ae Jeong, Jong Youl Lee, Kyung-ah Park, Kyung Eun Kim, Jung Eun Lee, Hyun-Jin Kim, Jong Ryeal Hahm, Gu Seob Roh, Jonathan M Peterson
PLOS ONE.2018; 13(7): e0200336. CrossRef - Cucurbita ficifolia (Cucurbitaceae) modulates inflammatory cytokines and IFN-γ in obese mice
Á. Fortis-Barrera, R. García-Macedo, J.C. Almanza-Perez, G. Blancas-Flores, A. Zamilpa-Alvarez, J.L. Flores-Sáenz, M. Cruz, R. Román-Ramos, F.J. Alarcón-Aguilar
Canadian Journal of Physiology and Pharmacology.2017; 95(2): 170. CrossRef - Lobeglitazone, a Novel Thiazolidinedione, Improves Non-Alcoholic Fatty Liver Disease in Type 2 Diabetes: Its Efficacy and Predictive Factors Related to Responsiveness
Yong-ho Lee, Jae Hyeon Kim, So Ra Kim, Heung Yong Jin, Eun-Jung Rhee, Young Min Cho, Byung-Wan Lee
Journal of Korean Medical Science.2017; 32(1): 60. CrossRef -
Peroxisome proliferator‐activated receptor‐γ agonists attenuate biofilm formation by
Pseudomonas aeruginosa
Brahmchetna Bedi, Nicholas M. Maurice, Vincent T. Ciavatta, K. Sabrina Lynn, Zhihong Yuan, Samuel A. Molina, Myungsoo Joo, William R. Tyor, Joanna B. Goldberg, Michael Koval, C. Michael Hart, Ruxana T. Sadikot
The FASEB Journal.2017; 31(8): 3608. CrossRef - Pioglitazone and the secondary prevention of cardiovascular disease. A meta-analysis of randomized-controlled trials
Marit de Jong, H. Bart van der Worp, Yolanda van der Graaf, Frank L. J. Visseren, Jan Westerink
Cardiovascular Diabetology.2017;[Epub] CrossRef - Gestational diabetes mellitus was related to ambient air pollutant nitric oxide during early gestation
Shih-Chun Pan, Ching-Chun Huang, Shio-Jean Lin, Bing-Yu Chen, Chang-Chuan Chan, Yue-Liang Leon Guo
Environmental Research.2017; 158: 318. CrossRef - The Multifaceted Haptoglobin in the Context of Adipose Tissue and Metabolism
Margherita Maffei, Ilaria Barone, Gaia Scabia, Ferruccio Santini
Endocrine Reviews.2016; 37(4): 403. CrossRef - Enhanced Clearance of Pseudomonas aeruginosa by Peroxisome Proliferator-Activated Receptor Gamma
Brahmchetna Bedi, Zhihong Yuan, Myungsoo Joo, Susu M. Zughaier, Joanna B. Goldberg, Jack L. Arbiser, C. Michael Hart, Ruxana T. Sadikot, B. A. McCormick
Infection and Immunity.2016; 84(7): 1975. CrossRef - F-box only protein 9 is an E3 ubiquitin ligase of PPARγ
Kyeong Won Lee, Soo Heon Kwak, Young Do Koo, Yun-Kyung Cho, Hak Mo Lee, Hye Seung Jung, Young Min Cho, Young Joo Park, Sung Soo Chung, Kyong Soo Park
Experimental & Molecular Medicine.2016; 48(5): e234. CrossRef - The Resin fromProtium heptaphyllumPrevents High-Fat Diet-Induced Obesity in Mice: Scientific Evidence and Potential Mechanisms
Karine Maria Martins Bezerra Carvalho, José Delano Barreto Marinho Filho, Tiago Sousa de Melo, Ana Jérsia Araújo, Josiane da Silva Quetz, Maria do Perpétuo Socorro Saldanha da Cunha, Karina Moura de Melo, Armenio Andre de Carvalho Almeida da Silva, Adrian
Evidence-Based Complementary and Alternative Medicine.2015; 2015: 1. CrossRef - Lobeglitazone and pioglitazone as add‐ons to metformin for patients with type 2 diabetes: a 24‐week, multicentre, randomized, double‐blind, parallel‐group, active‐controlled, phase III clinical trial with a 28‐week extension
S.‐M. Jin, C.‐Y. Park, Y. M. Cho, B. J. Ku, C. W. Ahn, B.‐S. Cha, K. W. Min, Y. A. Sung, S. H. Baik, K. W. Lee, K.‐H. Yoon, M.‐K. Lee, S. W. Park
Diabetes, Obesity and Metabolism.2015; 17(6): 599. CrossRef - Deconvolution of Complex 1D NMR Spectra Using Objective Model Selection
Travis S. Hughes, Henry D. Wilson, Ian Mitchelle S. de Vera, Douglas J. Kojetin, Paul C. Driscoll
PLOS ONE.2015; 10(8): e0134474. CrossRef - PPARγ partial agonist GQ-16 strongly represses a subset of genes in 3T3-L1 adipocytes
Flora Aparecida Milton, Aleksandra Cvoro, Angelica A. Amato, Douglas H. Sieglaff, Carly S. Filgueira, Anithachristy Sigamani Arumanayagam, Maria do Carmo Alves de Lima, Ivan Rocha Pitta, Francisco de Assis Rocha Neves, Paul Webb
Biochemical and Biophysical Research Communications.2015; 464(3): 718. CrossRef - Voluntary exercise prevents colonic inflammation in high-fat diet-induced obese mice by up-regulating PPAR-γ activity
Wei-Xin Liu, Ting Wang, Feng Zhou, Ying Wang, Jun-Wei Xing, Shen Zhang, Shou-Zhi Gu, Li-Xuan Sang, Cong Dai, Hai-Lan Wang
Biochemical and Biophysical Research Communications.2015; 459(3): 475. CrossRef - Effect of a new PPAR-gamma agonist, lobeglitazone, on neointimal formation after balloon injury in rats and the development of atherosclerosis
Soo Lim, Kuy-Sook Lee, Jie Eun Lee, Ho Seon Park, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Young Bum Kim, Hak Chul Jang
Atherosclerosis.2015; 243(1): 107. CrossRef - Antidiabetic agents: Potential anti-inflammatory activity beyond glucose control
A.J. Scheen, N. Esser, N. Paquot
Diabetes & Metabolism.2015; 41(3): 183. CrossRef - Genomic binding and regulation of gene expression by the thyroid carcinoma-associated PAX8-PPARG fusion protein
Yanxiao Zhang, Jingcheng Yu, Chee Lee, Bin Xu, Maureen A. Sartor, Ronald J. Koenig
Oncotarget.2015; 6(38): 40418. CrossRef - Peroxisome Proliferator-Activated Receptor γ (PPARγ) and Ligand Choreography: Newcomers Take the Stage
Santiago Garcia-Vallvé, Laura Guasch, Sarah Tomas-Hernández, Josep Maria del Bas, Vincent Ollendorff, Lluís Arola, Gerard Pujadas, Miquel Mulero
Journal of Medicinal Chemistry.2015; 58(14): 5381. CrossRef - Pathway Analysis of Metabolic Syndrome Using a Genome-Wide Association Study of Korea Associated Resource (KARE) Cohorts
Unjin Shim, Han-Na Kim, Yeon-Ah Sung, Hyung-Lae Kim
Genomics & Informatics.2014; 12(4): 195. CrossRef - Pax-8–PPAR-γ fusion protein in thyroid carcinoma
Priyadarshini Raman, Ronald J. Koenig
Nature Reviews Endocrinology.2014; 10(10): 616. CrossRef - Insulin therapy and colorectal cancer risk among type 2 diabetes mellitus patients: a systemic review and meta-analysis
Shinan Yin, Hua Bai, Danqing Jing
Diagnostic Pathology.2014;[Epub] CrossRef - Common biological mechanisms between bipolar disorder and type 2 diabetes: Focus on inflammation
Ajaykumar N. Sharma, Isabelle E. Bauer, Marsal Sanches, Juan F. Galvez, Giovana B. Zunta-Soares, Joao Quevedo, Flavio Kapczinski, Jair C. Soares
Progress in Neuro-Psychopharmacology and Biological Psychiatry.2014; 54: 289. CrossRef
- Lysine 222 in PPAR γ1 functions as the key site of MuRF2-mediated ubiquitination modification
- Effects of Sulfonylureas on Peroxisome Proliferator-Activated Receptor γ Activity and on Glucose Uptake by Thiazolidinediones
- Kyeong Won Lee, Yun Hyi Ku, Min Kim, Byung Yong Ahn, Sung Soo Chung, Kyong Soo Park
- Diabetes Metab J. 2011;35(4):340-347. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.340
- 4,289 View
- 41 Download
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Sulfonylurea primarily stimulates insulin secretion by binding to its receptor on the pancreatic β-cells. Recent studies have suggested that sulfonylureas induce insulin sensitivity through peroxisome proliferator-activated receptor γ (PPARγ), one of the nuclear receptors. In this study, we investigated the effects of sulfonylurea on PPARγ transcriptional activity and on the glucose uptake via PPARγ.
Methods Transcription reporter assays using Cos7 cells were performed to determine if specific sulfonylureas stimulate PPARγ transactivation. Glimepiride, gliquidone, and glipizide (1 to 500 µM) were used as treatment, and rosiglitazone at 1 and 10 µM was used as a control. The effects of sulfonylurea and rosiglitazone treatments on the transcriptional activity of endogenous PPARγ were observed. In addition, 3T3-L1 adipocytes were treated with rosiglitazone (10 µM), glimepiride (100 µM) or both to verify the effect of glimepiride on rosiglitazone-induced glucose uptake.
Results Sulfonylureas, including glimepiride, gliquidone and glipizide, increased PPARγ transcriptional activity, gliquidone being the most potent PPARγ agonist. However, no additive effects were observed in the presence of rosiglitazone. When rosiglitazone was co-treated with glimepiride, PPARγ transcriptional activity and glucose uptake were reduced compared to those after treatment with rosiglitazone alone. This competitive effect of glimepiride was observed only at high concentrations that are not achieved with clinical doses.
Conclusion Sulfonylureas like glimepiride, gliquidone and glipizide increased the transcriptional activity of PPARγ. Also, glimepiride was able to reduce the effect of rosiglitazone on PPARγ agonistic activity and glucose uptake. However, the competitive effect does not seem to occur at clinically feasible concentrations.
-
Citations
Citations to this article as recorded by- Chitosan-Encapsulated Nano-selenium Targeting TCF7L2, PPARγ, and CAPN10 Genes in Diabetic Rats
Omayma A. R. Abozaid, Sawsan M. El-Sonbaty, Neama M. A. Hamam, Moustafa A. Farrag, Ahmad S. Kodous
Biological Trace Element Research.2023; 201(1): 306. CrossRef - Insights from insulin resistance pathways: Therapeutic approaches against Alzheimer associated diabetes mellitus
Ayesha Fauzi, Ewen Se Thoe, Tang Yin Quan, Adeline Chia Yoke Yin
Journal of Diabetes and its Complications.2023; 37(11): 108629. CrossRef - Novel Sulfonanilide Inhibitors of SHIP2 Enhance Glucose Uptake into Cultured Myotubes
Mika E. A. Berg, Jette-Britt Naams, Laura C. Hautala, Tuomas A. Tolvanen, Jari P. Ahonen, Sanna Lehtonen, Kristiina Wähälä
ACS Omega.2020; 5(3): 1430. CrossRef - Diabetic Theory in Anti-Alzheimer’s Drug Research and Development - Part 1: Therapeutic Potential of Antidiabetic Agents
Agnieszka Jankowska, Anna Wesołowska, Maciej Pawłowski, Grażyna Chłoń-Rzepa
Current Medicinal Chemistry.2020; 27(39): 6658. CrossRef - Moringa concanensis Nimmo extracts ameliorates hyperglycemia-mediated oxidative stress and upregulates PPARγ and GLUT4 gene expression in liver and pancreas of streptozotocin-nicotinamide induced diabetic rats
Brindha Banu Balakrishnan, Kalaivani Krishnasamy, Vijayakumar Mayakrishnan, Arokiyaraj Selvaraj
Biomedicine & Pharmacotherapy.2019; 112: 108688. CrossRef - PPARγ Agonistic Activity of Sulphonylureas
Debjani Banerjee, Harnovdeep Singh Bharaj, Moulinath Banerjee
Endocrine, Metabolic & Immune Disorders - Drug Targets.2019; 19(4): 467. CrossRef - Glimepiride treatment in a patient with type A insulin resistance syndrome due to a novel heterozygous missense mutation in the insulin receptor gene
Zhimin Huang, Juan Liu, Kaka Ng, Xuesi Wan, Lijuan Xu, Xiaoying He, Zhihong Liao, Yanbing Li
Journal of Diabetes Investigation.2018; 9(5): 1075. CrossRef - Arsenic, Cadmium, and Lead Like Troglitazone Trigger PPARγ-Dependent Poly (ADP-Ribose) Polymerase Expression and Subsequent Apoptosis in Rat Brain Astrocytes
Rajesh Kushwaha, Juhi Mishra, Sachin Tripathi, Puneet Khare, Sanghamitra Bandyopadhyay
Molecular Neurobiology.2018; 55(3): 2125. CrossRef - Docosahexaenoic acid up‐regulates both PI3K/AKT‐dependent FABP7–PPARγ interaction and MKP3 that enhance GFAP in developing rat brain astrocytes
Sachin Tripathi, Rajesh Kushwaha, Juhi Mishra, Manoj Kumar Gupta, Harish Kumar, Somali Sanyal, Dhirendra Singh, Sabyasachi Sanyal, Amogh Anant Sahasrabuddhe, Mohan Kamthan, Mohana Krishna Reddy Mudiam, Sanghamitra Bandyopadhyay
Journal of Neurochemistry.2017; 140(1): 96. CrossRef - Antiglycation and cell protective actions of metformin and glipizide in erythrocytes and monocytes
Krishna Adeshara, Rashmi Tupe
Molecular Biology Reports.2016; 43(3): 195. CrossRef - The therapeutic journey of pyridazinone
Wasim Akhtar, M. Shaquiquzzaman, Mymoona Akhter, Garima Verma, Mohemmed Faraz Khan, M. Mumtaz Alam
European Journal of Medicinal Chemistry.2016; 123: 256. CrossRef - Antidiabetic effect of novel benzenesulfonylureas as PPAR-γ agonists and their anticancer effect
Chetna Kharbanda, Mohammad Sarwar Alam, Hinna Hamid, Kalim Javed, Abhijeet Dhulap, Sameena Bano, Yakub Ali
Bioorganic & Medicinal Chemistry Letters.2015; 25(20): 4601. CrossRef - Method Development and Validation of Amlodipine, Gliquidone and Pioglitazone: Application in the Analysis of Human Serum
Agha Zeeshan Mirza, M. Saeed Arayne, Najma Sultana
Analytical Chemistry Letters.2014; 4(5-6): 302. CrossRef - Gliquidone decreases urinary protein by promoting tubular reabsorption in diabetic Goto-Kakizaki rats
Jian-Ting Ke, Mi Li, Shi-Qing Xu, Wen-Jian Zhang, Yong-Wei Jiang, Lan-yun Cheng, Li Chen, Jin-Ning Lou, Wei Wu
Journal of Endocrinology.2014; 220(2): 129. CrossRef - Extension of Drosophila lifespan by cinnamon through a sex-specific dependence on the insulin receptor substrate chico
Samuel E. Schriner, Steven Kuramada, Terry E. Lopez, Stephanie Truong, Andrew Pham, Mahtab Jafari
Experimental Gerontology.2014; 60: 220. CrossRef - Crif1 Deficiency Reduces Adipose OXPHOS Capacity and Triggers Inflammation and Insulin Resistance in Mice
Min Jeong Ryu, Soung Jung Kim, Yong Kyung Kim, Min Jeong Choi, Surendar Tadi, Min Hee Lee, Seong Eun Lee, Hyo Kyun Chung, Saet Byel Jung, Hyun-Jin Kim, Young Suk Jo, Koon Soon Kim, Sang-Hee Lee, Jin Man Kim, Gi Ryang Kweon, Ki Cheol Park, Jung Uee Lee, Yo
PLoS Genetics.2013; 9(3): e1003356. CrossRef - Glimepiride attenuates Aβ production via suppressing BACE1 activity in cortical neurons
Feiyang Liu, Yijin Wang, Ming Yan, Luyong Zhang, Tao Pang, Hong Liao
Neuroscience Letters.2013; 557: 90. CrossRef - Pharmacologic agents for type 2 diabetes therapy and regulation of adipogenesis
A. Cignarelli, F. Giorgino, R. Vettor
Archives of Physiology and Biochemistry.2013; 119(4): 139. CrossRef - Labisia pumilaUpregulates Peroxisome Proliferator-Activated Receptor Gamma Expression in Rat Adipose Tissues and 3T3-L1 Adipocytes
Fazliana Mansor, Harvest F. Gu, Claes-Göran Östenson, Louise Mannerås-Holm, Elisabet Stener-Victorin, Wan Nazaimoon Wan Mohamud
Advances in Pharmacological Sciences.2013; 2013: 1. CrossRef - Protocol for effective differentiation of 3T3-L1 cells to adipocytes
Katja Zebisch, Valerie Voigt, Martin Wabitsch, Matthias Brandsch
Analytical Biochemistry.2012; 425(1): 88. CrossRef
- Chitosan-Encapsulated Nano-selenium Targeting TCF7L2, PPARγ, and CAPN10 Genes in Diabetic Rats
- Diabetes and Osteoporosis.
- Ki Won Oh
- Korean Diabetes J. 2009;33(3):169-177. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.169
- 1,936 View
- 22 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Increased life expectancy and increased obesity have contributed to an increasing incidence of osteoporosis and diabetes mellitus. Recent meta-analyses and cohort studies confirm that diabetes is associated with a higher risk of fracture. Patients with type 2 diabetes exhibit increased fracture risks despite a higher bone mass, which are mainly attributable to non-skeletal risk factors. Patients with type 1 diabetes may have impaired bone formation because of absence of the anabolic effects of insulin and insulin-like growth factor I (IGF-I) system. Several clinical studies have reported adverse skeletal actions of peroxisome proliferator-activated receptor gamma (PPARgamma) agonist in humans. Obesity regulates bone metabolism not only by increasing weight loading but also by modulating adipokines that are known to affect bone remodeling.
-
Citations
Citations to this article as recorded by- Relationship between hs-CRP and HbA1c in Diabetes Mellitus Patients: 2015–2017 Korean National Health and Nutrition Examination Survey
Yo-Han Seo, Hee-Young Shin
Chonnam Medical Journal.2021; 57(1): 62. CrossRef - Correlation between Serum Osteocalcin and Hemoglobin A1c in Gwangju General Hospital Patients
Yo-Han Seo, Hee-Young Shin
The Korean Journal of Clinical Laboratory Science.2018; 50(3): 313. CrossRef - Bergapten exerts inhibitory effects on diabetes-related osteoporosis via the regulation of the PI3K/AKT, JNK/MAPK and NF-κB signaling pathways in osteoprotegerin knockout mice
Xue-Ju Li, Zhe Zhu, Si-Lin Han, Zi-Long Zhang
International Journal of Molecular Medicine.2016; 38(6): 1661. CrossRef - The association of Osteoporosis and Thyroid Hormone in euthyroid adults
Hyun Yoon, Eun-Jin Ryu
Journal of the Korea Academia-Industrial cooperation Society.2015; 16(2): 1137. CrossRef - A Study on the Correlation between Menopausal Rating Scale and Bone Mineral Density for Menopausal Osteoporosis Patients
Kyu In Kwak, Jae Hui Kang, Yun Joo Kim, Hyun Lee
The Acupuncture.2014; 31(3): 25. CrossRef - Factors Associated with Bone Mineral Density in Korean Postmenopausal Women Aged 50 Years and Above: Using 2008-2010 Korean National Health and Nutrition Examination Survey
Son-Ok Mun, Jihye Kim, Yoon Jung Yang
Korean Journal of Community Nutrition.2013; 18(2): 177. CrossRef - Influencing Factors of Bone Mineral Density in Men
Dong-Ha Lee, Eun-Nam Lee
Journal of muscle and joint health.2011; 18(1): 5. CrossRef
- Relationship between hs-CRP and HbA1c in Diabetes Mellitus Patients: 2015–2017 Korean National Health and Nutrition Examination Survey

 KDA
KDA
 First
First Prev
Prev





