
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Temporal Changes in Resting Heart Rate and Risk of Diabetes Mellitus
- Mi Kyoung Son, Kyoungho Lee, Hyun-Young Park
- Received August 29, 2023 Accepted November 13, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0305 [Epub ahead of print]

- 605 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the association between the time-varying resting heart rate (RHR) and change in RHR (∆RHR) over time and the risk of diabetes mellitus (DM) by sex.
Methods
We assessed 8,392 participants without DM or atrial fibrillation/flutter from the Korean Genome and Epidemiology Study, a community-based prospective cohort study that was initiated in 2001 to 2002. The participants were followed up until December 31, 2018. Updating RHR with biennial in-study re-examinations, the time-varying ∆RHR was calculated by assessing the ∆RHR at the next follow-up visit.
Results
Over a median follow-up of 12.3 years, 1,345 participants (16.2%) had DM. As compared with RHR of 60 to 69 bpm, for RHR of ≥80 bpm, the incidence of DM was significantly increased for both male and female. A drop of ≥5 bpm in ∆RHR when compared with the stable ∆RHR group (–5< ∆RHR <5 bpm) was associated significantly with lower risk of DM in both male and female. However, an increase of ≥5 bpm in ∆RHR was significantly associated with higher risk of DM only in female, not in male (hazard ratio for male, 1.057 [95% confidence interval, 0.869 to 1.285]; and for female, 1.218 [95% confidence interval, 1.008 to 1.471]).
Conclusion
In this community-based longitudinal cohort study, a reduction in ∆RHR was associated with a decreased risk of DM, while an increase in ∆RHR was associated with an increased risk of DM only in female.
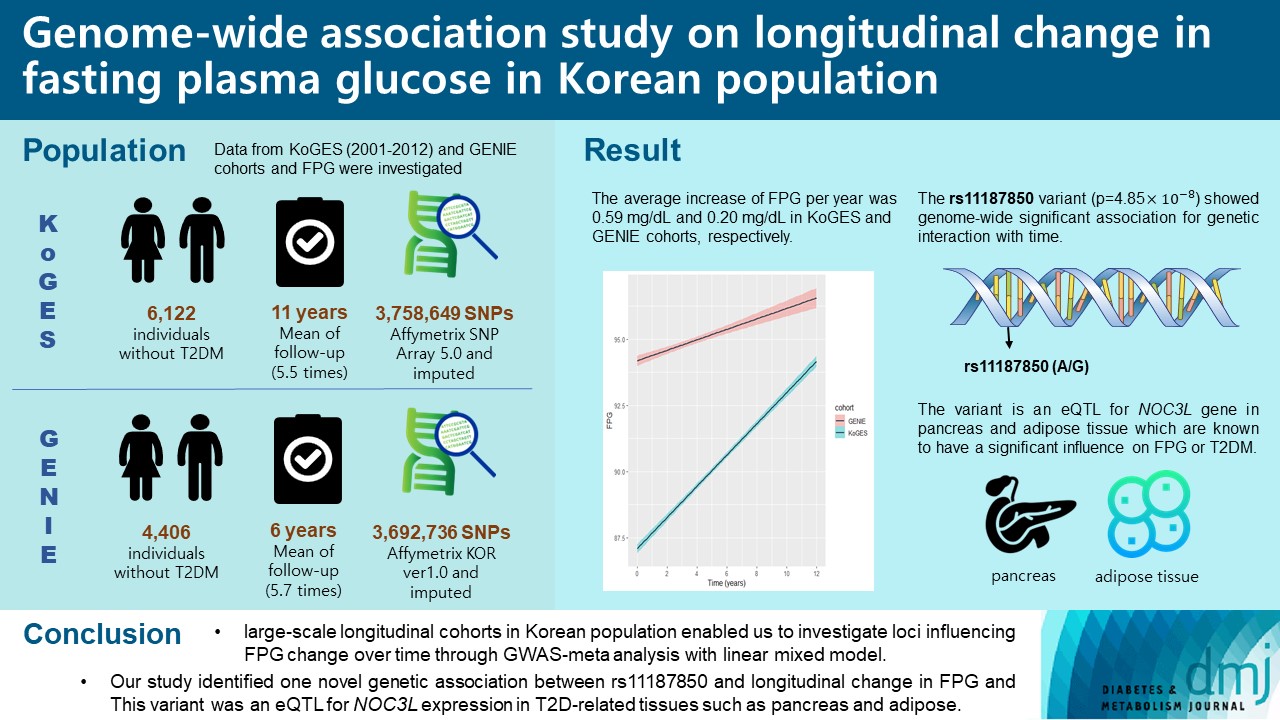
- Genetics
- Genome-Wide Association Study on Longitudinal Change in Fasting Plasma Glucose in Korean Population
- Heejin Jin, Soo Heon Kwak, Ji Won Yoon, Sanghun Lee, Kyong Soo Park, Sungho Won, Nam H. Cho
- Diabetes Metab J. 2023;47(2):255-266. Published online January 19, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0375
- 2,653 View
- 167 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Genome-wide association studies (GWAS) on type 2 diabetes mellitus (T2DM) have identified more than 400 distinct genetic loci associated with diabetes and nearly 120 loci for fasting plasma glucose (FPG) and fasting insulin level to date. However, genetic risk factors for the longitudinal deterioration of FPG have not been thoroughly evaluated. We aimed to identify genetic variants associated with longitudinal change of FPG over time.
Methods
We used two prospective cohorts in Korean population, which included a total of 10,528 individuals without T2DM. GWAS of repeated measure of FPG using linear mixed model was performed to investigate the interaction of genetic variants and time, and meta-analysis was conducted. Genome-wide complex trait analysis was used for heritability calculation. In addition, expression quantitative trait loci (eQTL) analysis was performed using the Genotype-Tissue Expression project.
Results
A small portion (4%) of the genome-wide single nucleotide polymorphism (SNP) interaction with time explained the total phenotypic variance of longitudinal change in FPG. A total of four known genetic variants of FPG were associated with repeated measure of FPG levels. One SNP (rs11187850) showed a genome-wide significant association for genetic interaction with time. The variant is an eQTL for NOC3 like DNA replication regulator (NOC3L) gene in pancreas and adipose tissue. Furthermore, NOC3L is also differentially expressed in pancreatic β-cells between subjects with or without T2DM. However, this variant was not associated with increased risk of T2DM nor elevated FPG level.
Conclusion
We identified rs11187850, which is an eQTL of NOC3L, to be associated with longitudinal change of FPG in Korean population.
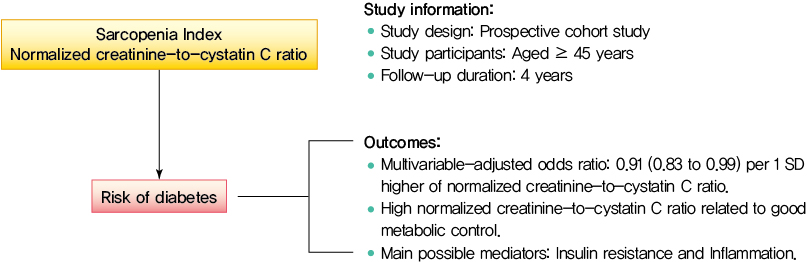
- Metabolic Risk/Epidemiology
- Normalized Creatinine-to-Cystatin C Ratio and Risk of Diabetes in Middle-Aged and Older Adults: The China Health and Retirement Longitudinal Study
- Shanhu Qiu, Xue Cai, Bo Xie, Yang Yuan, Zilin Sun, Tongzhi Wu
- Diabetes Metab J. 2022;46(3):476-485. Published online March 7, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0074
- 4,725 View
- 204 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Creatinine-to-cystatin C ratio is recently suggested to be a surrogate marker for sarcopenia. However, little is known about its association with diabetes. This study aimed to fill in this gap based on a large-scale prospective cohort.
Methods
A population-based representative sample of 5,055 participants aged ≥45 years from the China Health and Retirement Longitudinal Study was enrolled between 2011 and 2012 and followed at least once during the subsequent surveys at 2013, 2015, or 2018. Creatinine-to-cystatin C ratio was calculated and normalized by body weight. Incident diabetes was ascertained by plasma glucose, glycosylated hemoglobin, self-reported history, or use of anti-diabetic drugs. Logistic regression analysis and mediation analysis were employed.
Results
During follow-up, 634 participants developed diabetes. The risk of diabetes was gradually and significantly decreased with increased normalized creatinine–cystatin C ratio. The multivariable-adjusted odds ratio for diabetes was 0.91 (95% confidence interval, 0.83 to 0.99) per 1 standard deviation higher of normalized creatinine-to-cystatin C ratio, and this relationship remained significant after controlling for muscle strength. The risk reduction in diabetes was significantly larger in participants with normal-weight and high normalized creatinine-to-cystatin C ratio compared with those with overweight/obesity and high normalized creatinine-to-cystatin C ratio (Pinteraction=0.01). Insulin resistance and inflammation appeared to be key mediators accounting for the observed relationship between normalized creatinine-to-cystatin C ratio and risk of diabetes, with their mediating effect being 93.1% and 22.0%, respectively.
Conclusion
High normalized creatinine-to-cystatin C ratio is associated with reduced risk of diabetes in middle-aged and older adults. -
Citations
Citations to this article as recorded by- Muscle Quality in Relation to Prediabetes Phenotypes: A Population-Based Study With Mediation Analysis
Shanhu Qiu, Xue Cai, Xiaoying Zhou, Jinshui Xu, Zilin Sun, Haijian Guo, Tongzhi Wu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1151. CrossRef - Sex‐specific associations between skeletal muscle mass and incident diabetes: A population‐based cohort study
Dan Liu, Nan Li, Yiling Zhou, Miye Wang, Peige Song, Changzheng Yuan, Qingyang Shi, Hui Chen, Kaixin Zhou, Huan Wang, Tao Li, Xiong‐Fei Pan, Haoming Tian, Sheyu Li
Diabetes, Obesity and Metabolism.2024; 26(3): 820. CrossRef - Diabetes Mellitus Should Be Considered While Analysing Sarcopenia-Related Biomarkers
Justyna Rentflejsz, Zyta Beata Wojszel
Journal of Clinical Medicine.2024; 13(4): 1107. CrossRef - Associations of muscle mass and strength with new-onset diabetes among middle-aged and older adults: evidence from the China health and retirement longitudinal study (CHARLS)
Yun-Yun He, Mei-Ling Jin, Xiang-Yang Fang, Xiao-Juan Wang
Acta Diabetologica.2024;[Epub] CrossRef - The serum creatinine to cystatin C to waist circumference ratios predicts risk for type 2 diabetes: A Chinese cohort study
Yinfei Chen, Weiheng Wen, Zhiliang Mai, Ming Wang, Hong Chen, Jia Sun
Journal of Diabetes.2023; 15(10): 808. CrossRef - Associations of sarcopenia with peak expiratory flow among community-dwelling elderly population: based on the China Health and Retirement Longitudinal Study (CHARLS)
Yun-Yun He, Mei-Ling Jin, Jing Chang, Xiao-Juan Wang
European Geriatric Medicine.2023; 15(1): 95. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef
- Muscle Quality in Relation to Prediabetes Phenotypes: A Population-Based Study With Mediation Analysis
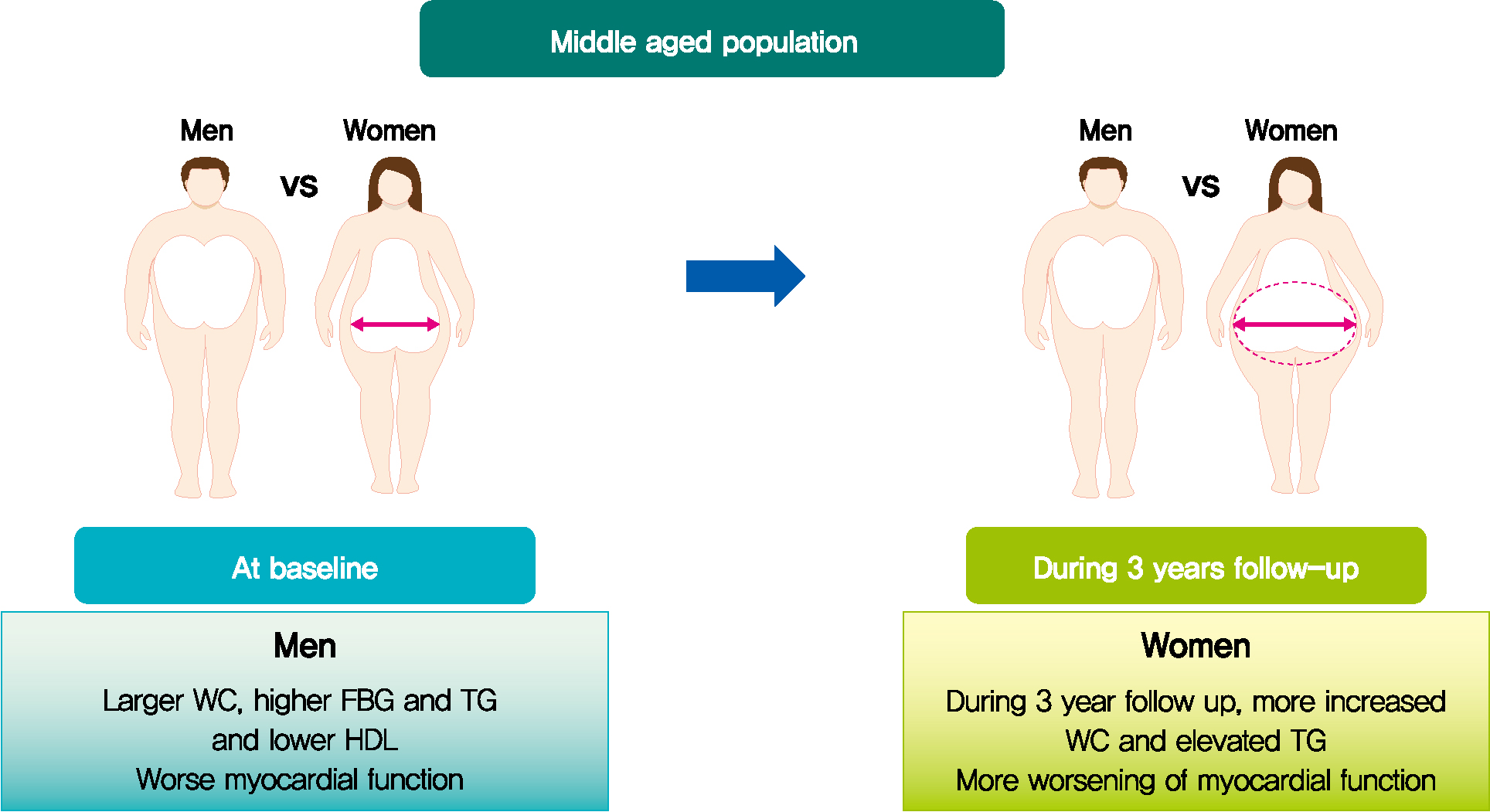
- Metabolic Risk/Epidemiology
- Longitudinal Change in Myocardial Function and Clinical Parameters in Middle-Aged Subjects: A 3-Year Follow-up Study
- Dong-Hyuk Cho, Hyung Joon Joo, Mi-Na Kim, Hee-Dong Kim, Do-Sun Lim, Seong-Mi Park
- Diabetes Metab J. 2021;45(5):719-729. Published online June 15, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0132
- 4,242 View
- 108 Download
- 2 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- Background
Metabolic syndrome (MetS) is closely associated with the aging process. However, changes in metabolic conditions and cardiac function that occur in middle aged population remain unclear. We evaluated longitudinal changes in metabolic parameters and cardiac function during a 3-year period in subjects with suspected MetS.
Methods
We studied 191 participants with suspected MetS at baseline and after 3 years. Anthropometric parameters, including waist circumference (WC), and metabolic parameters, including fasting blood glucose and lipid profile were measured. Conventional echocardiography with two-dimensional speckle tracking was performed.
Results
Mean age was 56.2±4.4 years, and there were 97 women (50.8%). Men had increased WC and triglycerides (TG) (WC 91.2±6.8 cm vs. 84.0±8.0 cm, P<0.001; TG 184.4±116.3 mg/dL vs. 128.2±53.6 mg/dL, P<0.001), and reduced global longitudinal strain (GLS) (–15.4%±2.1% vs. –17.1%±2.0%, P<0.001) compared to women. After 3.4 years, values of WC and TG did not change in men but increased in women (all P<0.05). The absolute value of left ventricular (LV) GLS did not change in men but was reduced in women (P=0.011). Change in TG was independently associated with worsening of LV GLS only in women (standardized β, –0.309; 95% confidence interval, –0.130 to –0.009; P=0.025).
Conclusion
In middle aged population, a vulnerable period for metabolic disturbance, cardiac remodeling tended to progress, which was prominent in women. Progression of adiposity and dyslipidemia after menopause may accelerate subclinical cardiac remodeling in middle-aged women. Lifestyle modification and medical interventions may help prevent further cardiac dysfunction in these subjects. -
Citations
Citations to this article as recorded by- Positive additive interaction effects of age, sex, obesity, and metabolic syndrome on left ventricular dysfunction
Dan Zhou, Zhongwen Ye, Zhiqiang Nie, Chaolei Chen, Songyuan Luo, Mengqi Yan, Jiabin Wang, Yingqing Feng
Journal of Diabetes.2024;[Epub] CrossRef - Lung-Heart Outcomes and Mortality through the 2020 COVID-19 Pandemic in a Prospective Cohort of Breast Cancer Radiotherapy Patients
Vincent Vinh-Hung, Olena Gorobets, Nele Adriaenssens, Hilde Van Parijs, Guy Storme, Dirk Verellen, Nam P. Nguyen, Nicolas Magne, Mark De Ridder
Cancers.2022; 14(24): 6241. CrossRef
- Positive additive interaction effects of age, sex, obesity, and metabolic syndrome on left ventricular dysfunction
- Obesity and Metabolic Syndrome
- The Protective Effects of Increasing Serum Uric Acid Level on Development of Metabolic Syndrome
- Tae Yang Yu, Sang-Man Jin, Jae Hwan Jee, Ji Cheol Bae, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2019;43(4):504-520. Published online February 21, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0079
- 4,711 View
- 52 Download
- 14 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background It has not been determined whether changes in serum uric acid (SUA) level are associated with incident metabolic syndrome (MetS). The aim of the current study was to investigate the relationship between changes in SUA level and development of MetS in a large number of subjects.
Methods In total, 13,057 subjects participating in a medical health check-up program without a diagnosis of MetS at baseline were enrolled. Cox proportional hazards models were used to test the independent association of percent changes in SUA level with development of MetS.
Results After adjustment for age, systolic blood pressure, body mass index, fat-free mass (%), estimated glomerular filtration rate, smoking status, fasting glucose, triglyceride, low density lipoprotein cholesterol, high density lipoprotein cholesterol, and baseline SUA levels, the hazard ratios (HRs) (95% confidence intervals [CIs]) for incident MetS in the second, third, and fourth quartiles compared to the first quartile of percent change in SUA level were 1.055 (0.936 to 1.190), 0.927 (0.818 to 1.050), and 0.807 (0.707 to 0.922) in male (
P for trend <0.001) and 1.000 (0.843 to 1.186), 0.744 (0.615 to 0.900), and 0.684 (0.557 to 0.840) in female (P for trend <0.001), respectively. As a continuous variable in the fully-adjusted model, each one-standard deviation increase in percent change in SUA level was associated with an HR (95% CI) for incident MetS of 0.944 (0.906 to 0.982) in male (P =0.005) and 0.851 (0.801 to 0.905) in female (P <0.001).Conclusion The current study demonstrated that increasing SUA level independently protected against the development of MetS, suggesting a possible role of SUA as an antioxidant in the pathogenesis of incident MetS.
-
Citations
Citations to this article as recorded by- High prevalence of hyperuricemia and the association with metabolic syndrome in the rural areas of Southwestern China: A structural equation modeling based on the Zhuang minority cohort
Xiaofen Tang, Shun Liu, Xiaoqiang Qiu, Li Su, Dongping Huang, Jun Liang, Yu Yang, Jennifer Hui Juan Tan, Xiaoyun Zeng, Yihong Xie
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(2): 497. CrossRef - Predictive Value of Collagen Biomarkers in Advanced Chronic Kidney Disease Patients
Carina Ureche, Gianina Dodi, Adela Mihaela Șerban, Andreea Simona Covic, Luminița Voroneanu, Simona Hogaș, Radu Andy Sascău, Cristian Stătescu, Adrian Covic
Biomolecules.2023; 13(2): 389. CrossRef - The bidirectional relationship between metabolic syndrome and hyperuricemia in China: A longitudinal study from CHARLS
Wen-Yu Chen, Yan-Peng Fu, Min Zhou
Endocrine.2022; 76(1): 62. CrossRef - Correlation between Serum Oxidative Stress Level and Serum Uric Acid and Prognosis in Patients with Hepatitis B-Related Liver Cancer before Operation
Maowen Yu, Chaozhu Zhang, Hongbo Tang, Chaohui Xiao, Hangjun Che
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - Association between metabolic syndrome and uric acid: a systematic review and meta-analysis
Elena Raya-Cano, Manuel Vaquero-Abellán, Rafael Molina-Luque, Domingo De Pedro-Jiménez, Guillermo Molina-Recio, Manuel Romero-Saldaña
Scientific Reports.2022;[Epub] CrossRef - Acute moderate‐intensity aerobic exercise promotes purinergic and inflammatory responses in sedentary, overweight and physically active subjects
Cesar Eduardo Jacintho Moritz, Franccesco Pinto Boeno, Alexandra Ferreira Vieira, Samuel Vargas Munhoz, Juliete Nathali Scholl, Amanda de Fraga Dias, Pauline Rafaela Pizzato, Fabrício Figueiró, Ana Maria Oliveira Battastini, Alvaro Reischak‐Oliveira
Experimental Physiology.2021; 106(4): 1024. CrossRef - Association between baseline and changes in serum uric acid and incident metabolic syndrome: a nation-wide cohort study and updated meta-analysis
Sen Chen, Nianwei Wu, Chuan Yu, Ying Xu, Chengfu Xu, Yuli Huang, Jian Zhao, Ningxiu Li, Xiong-Fei Pan
Nutrition & Metabolism.2021;[Epub] CrossRef - Can biomarkers be used to improve diagnosis and prediction of metabolic syndrome in childhood cancer survivors? A systematic review
Vincent G. Pluimakers, Selveta S. van Santen, Marta Fiocco, Marie‐Christine E. Bakker, Aart J. van der Lelij, Marry M. van den Heuvel‐Eibrink, Sebastian J. C. M. M. Neggers
Obesity Reviews.2021;[Epub] CrossRef - Inverse associations between serum urate and glycemic status in a general population and in persons with diabetes mellitus
Ichiro Wakabayashi
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Association of Serum Uric Acid with Metabolic Syndrome and Its Components: A Mendelian Randomization Analysis
Lu Wang, Tao Zhang, Yafei Liu, Fang Tang, Fuzhong Xue
BioMed Research International.2020; 2020: 1. CrossRef - Association between Serum Uric Acid and Metabolic Syndrome in Koreans
Jihyun Jeong, Young Ju Suh
Journal of Korean Medical Science.2019;[Epub] CrossRef
- High prevalence of hyperuricemia and the association with metabolic syndrome in the rural areas of Southwestern China: A structural equation modeling based on the Zhuang minority cohort
- Obesity and Metabolic Syndrome
- Utility of Serum Albumin for Predicting Incident Metabolic Syndrome According to Hyperuricemia
- You-Bin Lee, Ji Eun Jun, Seung-Eun Lee, Jiyeon Ahn, Gyuri Kim, Jae Hwan Jee, Ji Cheol Bae, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2018;42(6):529-537. Published online September 28, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0012
- 4,372 View
- 47 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Serum albumin and uric acid have been positively linked to metabolic syndrome (MetS). However, the association of MetS incidence with the combination of uric acid and albumin levels has not been investigated. We explored the association of albumin and uric acid with the risk of incident MetS in populations divided according to the levels of these two parameters.
Methods In this retrospective longitudinal study, 11,613 non-MetS participants were enrolled among 24,185 individuals who had undergone at least four annual check-ups between 2006 and 2012. The risk of incident MetS was analyzed according to four groups categorized by the sex-specific medians of serum albumin and uric acid.
Results During 55,407 person-years of follow-up, 2,439 cases of MetS developed. The risk of incident MetS increased as the uric acid category advanced in individuals with lower or higher serum albumin categories with hazard ratios (HRs) of 1.386 (95% confidence interval [CI], 1.236 to 1.554) or 1.314 (95% CI, 1.167 to 1.480). However, the incidence of MetS increased with higher albumin levels only in participants in the lower uric acid category with a HR of 1.143 (95% CI, 1.010 to 1.294).
Conclusion Higher levels of albumin were associated with an increased risk of incident MetS only in individuals with lower uric acid whereas higher levels of uric acid were positively linked to risk of incident MetS regardless of albumin level.
-
Citations
Citations to this article as recorded by- Dissecting the risk factors for hyperuricemia in vegetarians in Taiwan
Kai-Chieh Chang, Sin-Yi Huang, Wen-Hsin Tsai, Hao-Wen Liu, Jia-Sin Liu, Chia-Lin Wu, Ko-Lin Kuo
Journal of the Chinese Medical Association.2024; 87(4): 393. CrossRef - A predictive model for hyperuricemia among type 2 diabetes mellitus patients in Urumqi, China
Palizhati Abudureyimu, Yuesheng Pang, Lirun Huang, Qianqian Luo, Xiaozheng Zhang, Yifan Xu, Liang Jiang, Patamu Mohemaiti
BMC Public Health.2023;[Epub] CrossRef - Synergistic Interaction between Hyperuricemia and Abdominal Obesity as a Risk Factor for Metabolic Syndrome Components in Korean Population
Min Jin Lee, Ah Reum Khang, Yang Ho Kang, Mi Sook Yun, Dongwon Yi
Diabetes & Metabolism Journal.2022; 46(5): 756. CrossRef - Nutritional Biomarkers and Heart Rate Variability in Patients with Subacute Stroke
Eo Jin Park, Seung Don Yoo
Nutrients.2022; 14(24): 5320. CrossRef - Mean and visit-to-visit variability of glycemia and left ventricular diastolic dysfunction: A longitudinal analysis of 3025 adults with serial echocardiography
Jiyeon Ahn, Janghyun Koh, Darae Kim, Gyuri Kim, Kyu Yeon Hur, Sang Won Seo, Kyunga Kim, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
Metabolism.2021; 116: 154451. CrossRef - Can biomarkers be used to improve diagnosis and prediction of metabolic syndrome in childhood cancer survivors? A systematic review
Vincent G. Pluimakers, Selveta S. van Santen, Marta Fiocco, Marie‐Christine E. Bakker, Aart J. van der Lelij, Marry M. van den Heuvel‐Eibrink, Sebastian J. C. M. M. Neggers
Obesity Reviews.2021;[Epub] CrossRef - Heart Disease and Stroke Statistics—2020 Update: A Report From the American Heart Association
Salim S. Virani, Alvaro Alonso, Emelia J. Benjamin, Marcio S. Bittencourt, Clifton W. Callaway, April P. Carson, Alanna M. Chamberlain, Alexander R. Chang, Susan Cheng, Francesca N. Delling, Luc Djousse, Mitchell S.V. Elkind, Jane F. Ferguson, Myriam Forn
Circulation.2020;[Epub] CrossRef - Association between dairy product consumption and hyperuricemia in an elderly population with metabolic syndrome
Guillermo Mena-Sánchez, Nancy Babio, Nerea Becerra-Tomás, Miguel Á. Martínez-González, Andrés Díaz-López, Dolores Corella, Maria D. Zomeño, Dora Romaguera, Jesús Vioque, Ángel M. Alonso-Gómez, Julia Wärnberg, José A. Martínez, Luís Serra-Majem, Ramon Estr
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(2): 214. CrossRef - Evaluation of serum uric acid levels in patients with rosacea
Nermin Karaosmanoglu, Engin Karaaslan, Pınar Ozdemir Cetinkaya
Archives of Dermatological Research.2020; 312(6): 447. CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef
- Dissecting the risk factors for hyperuricemia in vegetarians in Taiwan
- Obesity and Metabolic Syndrome
- Serum Calcium and the Risk of Incident Metabolic Syndrome: A 4.3-Year Retrospective Longitudinal Study
- Jong Ha Baek, Sang-Man Jin, Ji Cheol Bae, Jae Hwan Jee, Tae Yang Yu, Soo Kyoung Kim, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2017;41(1):60-68. Published online December 26, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.60
- 4,073 View
- 32 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background An association between serum calcium level and risk of metabolic syndrome (MetS) has been suggested in cross-sectional studies. This study aimed to evaluate the association between baseline serum calcium level and risk of incident MetS in a longitudinal study.
Methods We conducted a retrospective longitudinal study of 12,706 participants without MetS who participated in a health screening program, had normal range serum calcium level at baseline (mean age, 51 years), and were followed up for 4.3 years (18,925 person-years). The risk of developing MetS was analyzed according to the baseline serum calcium levels.
Results A total of 3,448 incident cases (27.1%) of MetS developed during the follow-up period. The hazard ratio (HR) for incident MetS did not increase with increasing tertile of serum calcium level in an age- and sex-matched model (
P for trend=0.915). The HRs (95% confidence interval [CI]) for incident MetS comparing the second and the third tertiles to the first tertile of baseline serum calcium level were 0.91 (95% CI, 0.84 to 0.99) and 0.85 (95% CI, 0.78 to 0.92) in a fully adjusted model, respectively (P for trend=0.001). A decreased risk of incident MetS in higher tertiles of serum calcium level was observed in subjects with central obesity and/or a metabolically unhealthy state at baseline.Conclusion There was no positive correlation between baseline serum calcium levels and incident risk of MetS in this longitudinal study. There was an association between higher serum calcium levels and decreased incident MetS in individuals with central obesity or two components of MetS at baseline.
-
Citations
Citations to this article as recorded by- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018
Haolong Qi, Bin Wang, Lei Zhu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association of the serum calcium level with metabolic syndrome and its components among adults in Taiwan
Jer-min Chen, Tai-yin Wu, Yi-fan Wu, Kuan-liang Kuo
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Elevated Chinese visceral adiposity index increases the risk of stroke in Chinese patients with metabolic syndrome
Zeyu Liu, Qin Huang, Bi Deng, Minping Wei, Xianjing Feng, Fang Yu, Jie Feng, Yang Du, Jian Xia
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metformin: Expanding the Scope of Application—Starting Earlier than Yesterday, Canceling Later
Yulia A. Kononova, Nikolai P. Likhonosov, Alina Yu. Babenko
International Journal of Molecular Sciences.2022; 23(4): 2363. CrossRef - Metformin in prediabetes: key mechanisms for the prevention of diabetes and cardiometabolic risks
A. Yu. Babenko
Meditsinskiy sovet = Medical Council.2022; (10): 96. CrossRef Calcium and Phosphate Levels are Among Other Factors Associated with Metabolic Syndrome in Patients with Normal Weight
Kamila Osadnik, Tadeusz Osadnik, Marcin Delijewski, Mateusz Lejawa, Martyna Fronczek, Rafał Reguła, Mariusz Gąsior, Natalia Pawlas
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1281. CrossRef- Association between selected trace elements and body mass index and waist circumference: A cross sectional study
Mahnaz Zohal, Saeedeh Jam-Ashkezari, Nasim Namiranian, Amin Moosavi, Akram Ghadiri-Anari
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1293. CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef - Genotype effects of glucokinase regulator on lipid profiles and glycemic status are modified by circulating calcium levels: results from the Korean Genome and Epidemiology Study
Oh Yoen Kim, So-Young Kwak, Hyunjung Lim, Min-Jeong Shin
Nutrition Research.2018; 60: 96. CrossRef
- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018

 KDA
KDA
 First
First Prev
Prev





