
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Guideline/Fact Sheet
- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hypertension
- Jong Han Choi, Jee-Hyun Kang, Suk Chon
- Diabetes Metab J. 2022;46(3):377-390. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0051
- 5,013 View
- 250 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The Joint Committee of the Korean Diabetes Association, the Korean Society for the Study of Obesity, and the Korean Society of Hypertension announced a consensus statement on carbohydrate-restricted diets and intermittent fasting, representing an emerging and popular dietary pattern. In this statement, we recommend moderately-low-carbohydrate or low-carbohydrate diets, not a very-low-carbohydrate diet, for patients with type 2 diabetes mellitus. These diets can be considered a dietary regimen to improve glycemic control and reduce body weight in adults with type 2 diabetes mellitus. This review provides the detailed results of a meta-analysis and systematic literature review on the potential harms and benefits of carbohydrate-restricted diets in patients with diabetes. We expect that this review will help experts and patients by fostering an in-depth understanding and appropriate application of carbohydrate-restricted diets in the comprehensive management of diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
Do Gyeong Lee, In Gyeong Kang, Tae Seok Kim, Yun Ahn, Sang Yun Lee, Hye Jin Ahn, Yoo Kyoung Park
Nutrition.2024; 118: 112287. CrossRef - Long-Term Results of a Digital Diabetes Self-Management and Education Support Program Among Adults With Type 2 Diabetes: A Retrospective Cohort Study
Ashley Berthoumieux, Sarah Linke, Melinda Merry, Alison Megliola, Jessie Juusola, Jenna Napoleone
The Science of Diabetes Self-Management and Care.2024; 50(1): 19. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef
- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
- Guideline/Fact Sheet
- Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hypertension
- Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim, Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (KSSO), Committee of Clinical Practice Guidelines and Committee of Food and Nutrition, Korean Diabetes Association (KDA), Policy Committee of Korean Society of Hypertension (KSH), Policy Development Committee of National Academy of Medicine of Korea (NAMOK)
- Diabetes Metab J. 2022;46(3):355-376. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0038
- 11,121 View
- 588 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
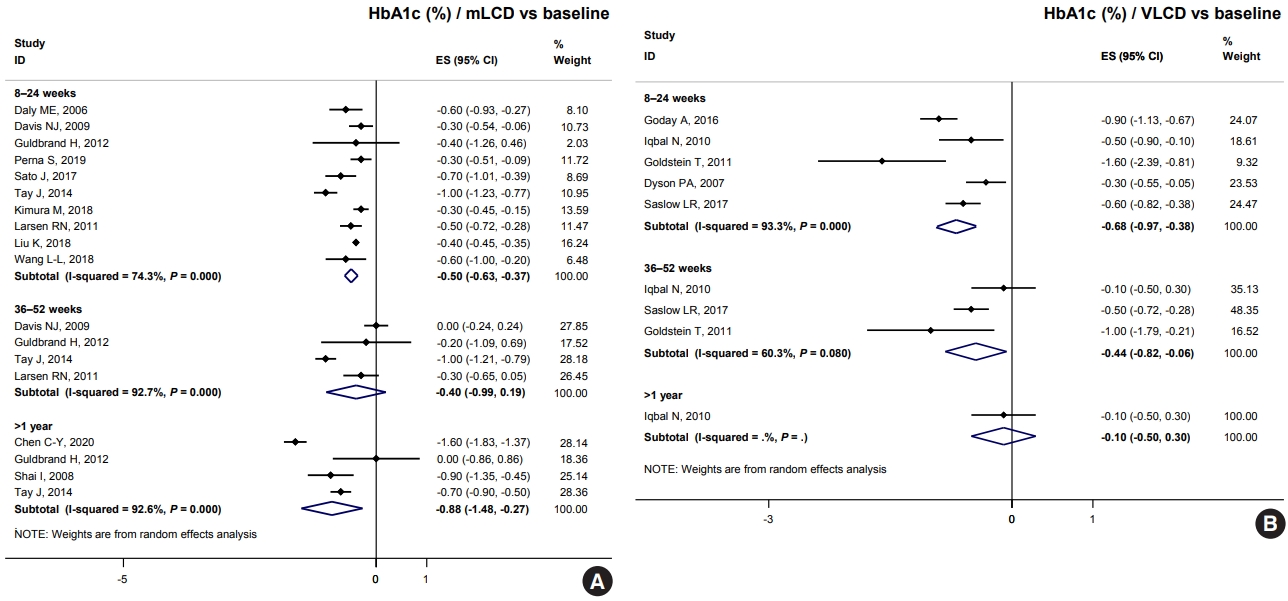
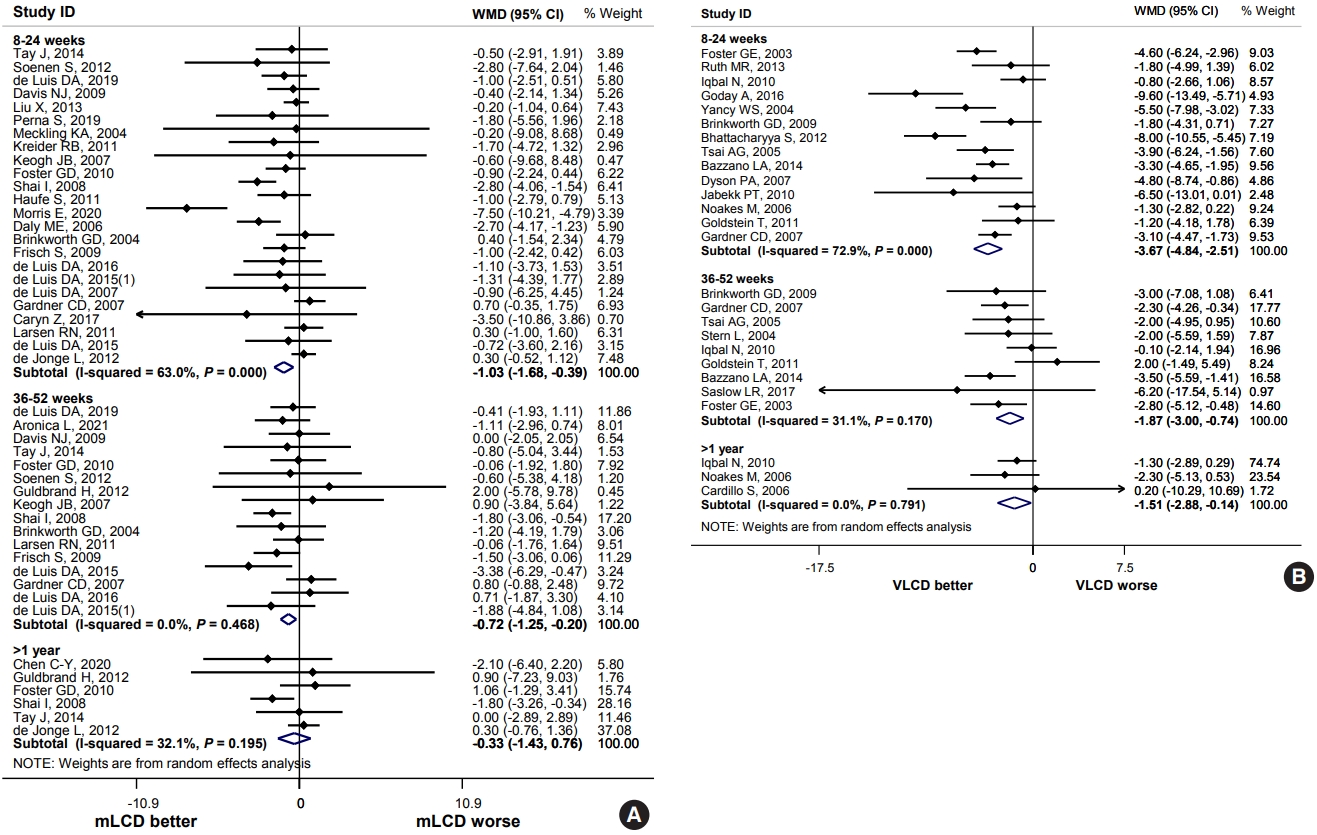
ePub - Carbohydrate-restricted diets and intermittent fasting (IF) have been rapidly gaining interest among the general population and patients with cardiometabolic disease, such as overweight or obesity, diabetes, and hypertension. However, there are limited expert recommendations for these dietary regimens. This study aimed to evaluate the level of scientific evidence on the benefits and harms of carbohydrate-restricted diets and IF to make responsible recommendations. A meta-analysis and systematic literature review of 66 articles on 50 randomized controlled trials (RCTs) of carbohydrate-restricted diets and 10 articles on eight RCTs of IF was performed. Based on the analysis, the following recommendations are suggested. In adults with overweight or obesity, a moderately-low carbohydrate or low carbohydrate diet (mLCD) can be considered as a dietary regimen for weight reduction. In adults with type 2 diabetes mellitus, mLCD can be considered as a dietary regimen for improving glycemic control and reducing body weight. In contrast, a very-low carbohydrate diet (VLCD) and IF are recommended against in patients with diabetes. Furthermore, no recommendations are suggested for VLCD and IF in adults with overweight or obesity, and carbohydrate-restricted diets and IF in patients with hypertension. Here, we describe the results of our analysis and the evidence for these recommendations.
-
Citations
Citations to this article as recorded by- Metabolic changes with intermittent fasting
Maria G. Lange, Alice A. Coffey, Paul C. Coleman, Thomas M. Barber, Thijs Van Rens, Oyinlola Oyebode, Sally Abbott, Petra Hanson
Journal of Human Nutrition and Dietetics.2024; 37(1): 256. CrossRef - Papel do Jejum Intermitente e da Dieta Restrita em Carboidratos na Prevenção de Doenças Cardiovasculares em Pacientes Pré-Diabéticos
Mohamed Khalfallah, Basma Elnagar, Shaimaa S. Soliman, Ahmad Eissa, Amany Allaithy
Arquivos Brasileiros de Cardiologia.2023;[Epub] CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Euglycemic diabetic ketoacidosis development in a patient with type 2 diabetes receiving a sodium-glucose cotransporter-2 inhibitor and a carbohydrate-restricted diet
Gwanpyo Koh, Jisun Bang, Soyeon Yoo, Sang Ah Lee
Journal of Medicine and Life Science.2023; 20(3): 126. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - The Related Metabolic Diseases and Treatments of Obesity
Ming Yang, Shuai Liu, Chunye Zhang
Healthcare.2022; 10(9): 1616. CrossRef - Updated Meta-Analysis of Studies from 2011 to 2021 Comparing the Effectiveness of Intermittent Energy Restriction and Continuous Energy Restriction
Kyoung-Kon Kim, Jee-Hyun Kang, Eun Mi Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(3): 230. CrossRef
- Metabolic changes with intermittent fasting
- Lifestyle
- Reducing Carbohydrate from Individual Sources Has Differential Effects on Glycosylated Hemoglobin in Type 2 Diabetes Mellitus Patients on Moderate Low-Carbohydrate Diets
- Hajime Haimoto, Shiho Watanabe, Keiko Maeda, Takashi Murase, Kenji Wakai
- Diabetes Metab J. 2021;45(3):390-403. Published online July 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0033
- 5,817 View
- 160 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 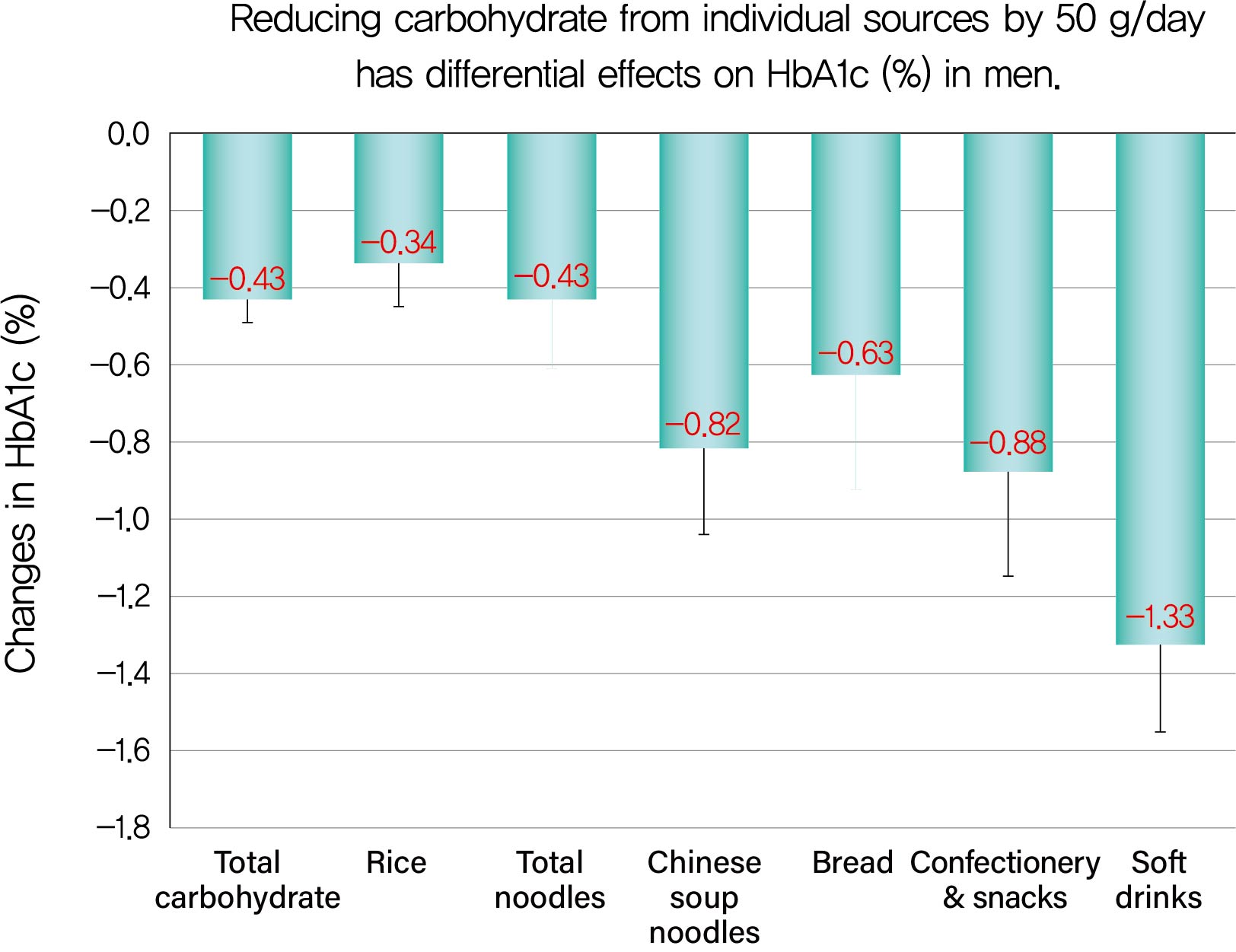
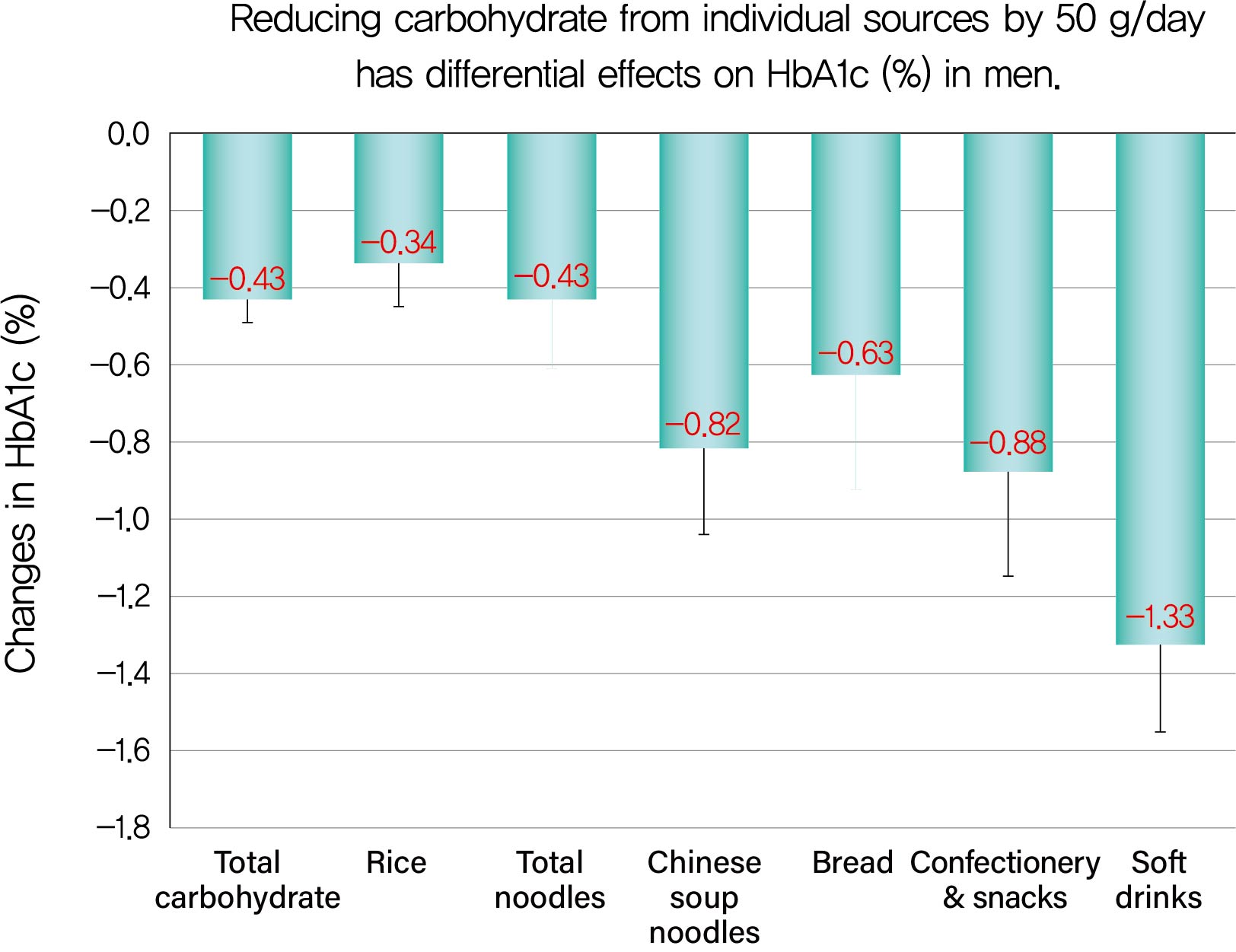
Background We evaluated decreases in glycosylated hemoglobin (HbA1c) achieved by reducing carbohydrate from various sources in type 2 diabetes mellitus patients.
Methods We followed up 138 male and 107 female outpatients on a moderate low-carbohydrate diet without diabetic medication for 6 months. Changes in carbohydrate sources (Δcarbohydrate) were assessed from 3-day dietary records at baseline and 6 months, and associations with changes in HbA1c (ΔHbA1c) were examined with Spearman's correlation coefficients (
r s) and multiple regression analysis.Results ΔHbA1c was −1.5%±1.6% in men and −0.9%±1.3% in women, while Δtotal carbohydrate was −115.3±103.7 g/day in men and −63.6±71.1 g/day in women. Positive associations with ΔHbA1c were found for Δtotal carbohydrate (
r s=0.584), Δcarbohydrate from soft drinks (0.368), confectionery (0.361), rice (0.325), bread (0.221), Chinese soup noodles (0.199) in men, and Δtotal carbohydrate (0.547) and Δcarbohydrate from rice (0.376) and confectionery (0.195) in women. Reducing carbohydrate sources by 50 g achieved decreases in HbA1c of 0.43% for total carbohydrate, 1.33% for soft drinks, 0.88% for confectionery, 0.63% for bread, 0.82% for Chinese soup noodles and 0.34% for rice in men and 0.45% for total carbohydrate, 0.67% for confectionery and 0.34% for rice in women, although mean reductions in carbohydrate from these sources were much smaller than that from rice.Conclusion Decreases in HbA1c achieved by reducing carbohydrate from soft drinks, confectionery, bread and Chinese soup noodles were 2- to 4-fold greater than that for rice. Our results will enable patients to decrease HbA1c efficiently (UMIN000009866).
-
Citations
Citations to this article as recorded by- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
Rashmeet Toor, Inderveer Chana
Medical & Biological Engineering & Computing.2022; 60(4): 991. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef
- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach

 KDA
KDA
 First
First Prev
Prev





