
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
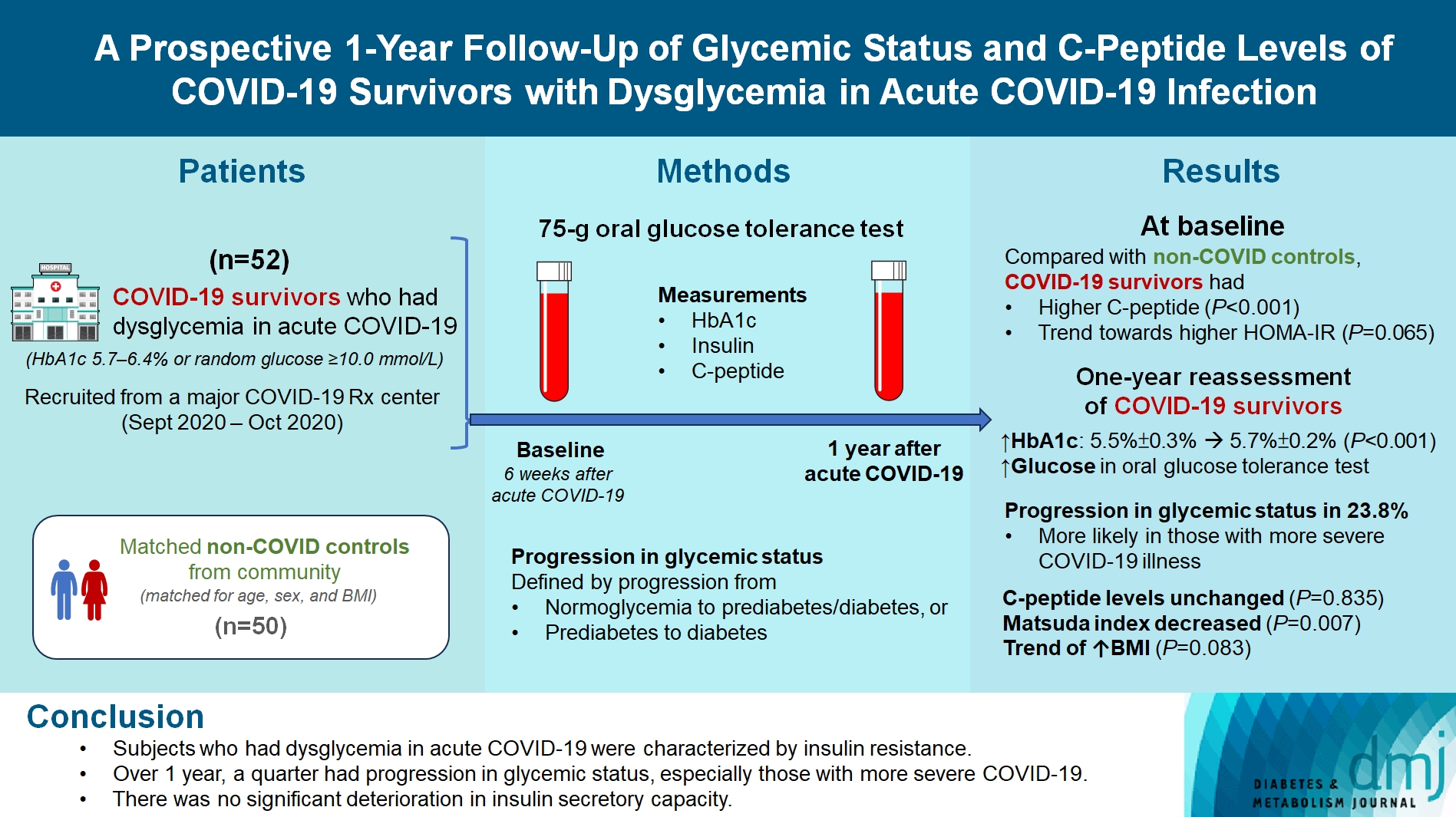
- A Prospective 1-Year Follow-Up of Glycemic Status and C-Peptide Levels of COVID-19 Survivors with Dysglycemia in Acute COVID-19 Infection
- David Tak Wai Lui, Chi Ho Lee, Ying Wong, Carol Ho Yi Fong, Kimberly Hang Tsoi, Yu Cho Woo, Kathryn Choon Beng Tan
- Received June 5, 2023 Accepted October 13, 2023 Published online March 11, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0175 [Epub ahead of print]
- 795 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
We evaluated changes in glycemic status, over 1 year, of coronavirus disease 2019 (COVID-19) survivors with dysglycemia in acute COVID-19.
Methods
COVID-19 survivors who had dysglycemia (defined by glycosylated hemoglobin [HbA1c] 5.7% to 6.4% or random glucose ≥10.0 mmol/L) in acute COVID-19 were recruited from a major COVID-19 treatment center from September to October 2020. Matched non-COVID controls were recruited from community. The 75-g oral glucose tolerance test (OGTT) were performed at baseline (6 weeks after acute COVID-19) and 1 year after acute COVID-19, with HbA1c, insulin and C-peptide measurements. Progression in glycemic status was defined by progression from normoglycemia to prediabetes/diabetes, or prediabetes to diabetes.
Results
Fifty-two COVID-19 survivors were recruited. Compared with non-COVID controls, they had higher C-peptide (P< 0.001) and trend towards higher homeostasis model assessment of insulin resistance (P=0.065). Forty-three COVID-19 survivors attended 1-year reassessment. HbA1c increased from 5.5%±0.3% to 5.7%±0.2% (P<0.001), with increases in glucose on OGTT at fasting (P=0.089), 30-minute (P=0.126), 1-hour (P=0.014), and 2-hour (P=0.165). At baseline, 19 subjects had normoglycemia, 23 had prediabetes, and one had diabetes. Over 1 year, 10 subjects (23.8%; of 42 non-diabetes subjects at baseline) had progression in glycemic status. C-peptide levels remained unchanged (P=0.835). Matsuda index decreased (P=0.007) and there was a trend of body mass index increase from 24.4±2.7 kg/m2 to 25.6±5.2 (P=0.083). Subjects with progression in glycemic status had more severe COVID-19 illness than non-progressors (P=0.030). Reassessment was not performed in the control group.
Conclusion
Subjects who had dysglycemia in acute COVID-19 were characterized by insulin resistance. Over 1 year, a quarter had progression in glycemic status, especially those with more severe COVID-19. Importantly, there was no significant deterioration in insulin secretory capacity.
- Others
- Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
- Insa Laspe, Juris J. Meier, Michael A. Nauck
- Diabetes Metab J. 2023;47(1):140-146. Published online March 22, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0322
- 65,535 View
- 184 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
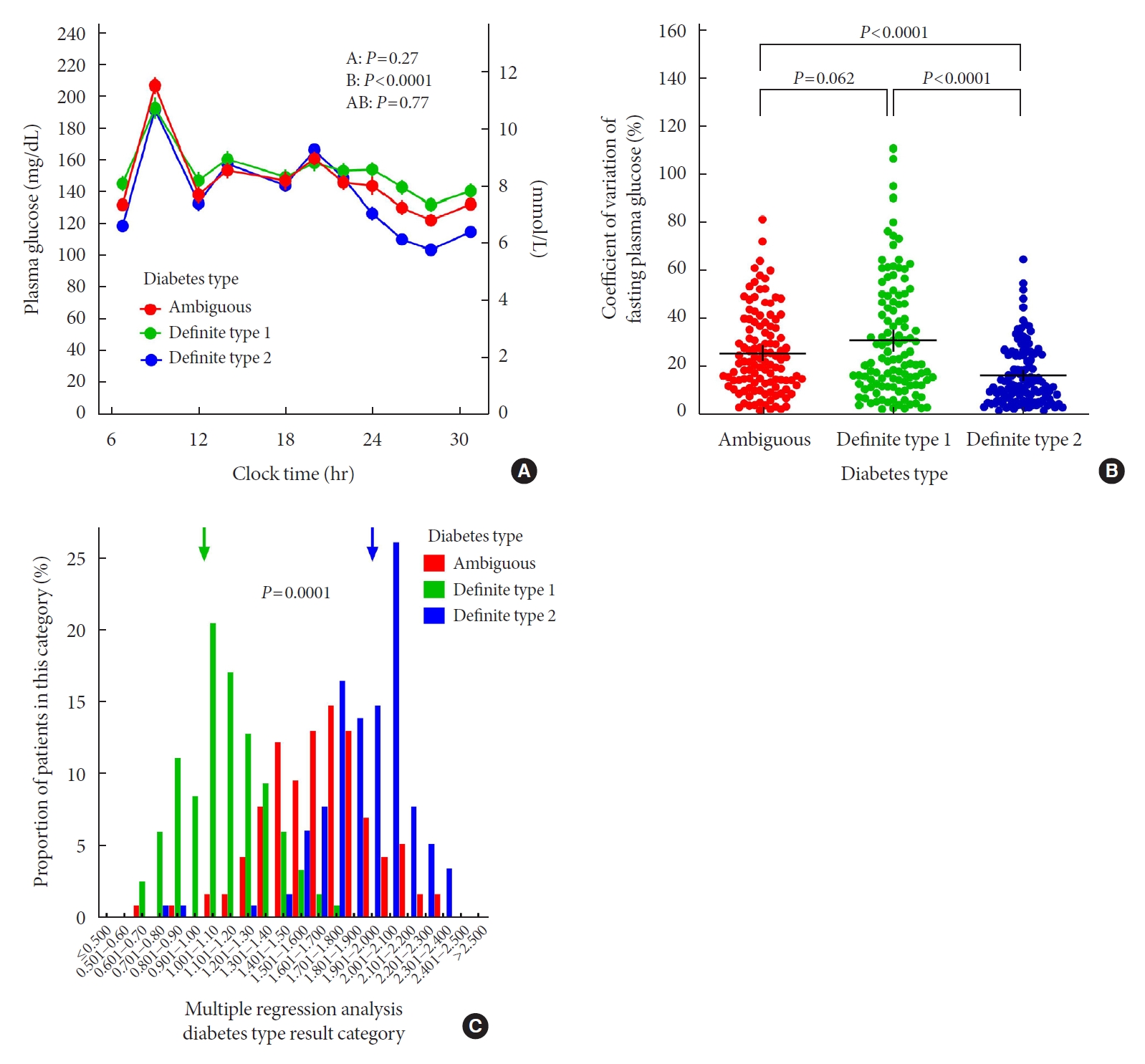
ePub - In clinical practice, the distinction between type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) can be challenging, leaving patients with “ambiguous” diabetes type. Insulin-treated patients (n=115) previously diagnosed with T2DM had to be re-classified based on clinical phenotype and laboratory results, and were operationally defined as having an ambiguous diabetes type. They were compared against patients with definite T1DM and T2DM regarding 12 clinical and laboratory features typically different between diabetes types. Characteristics of patients with ambiguous diabetes type, representing approximately 6% of all patients with T1DM or T2DM seen at our specialized clinic, fell in between those of patients with definite T1DM and T2DM, both regarding individual features and with respect to a novel classification based on multi-variable regression analysis (P<0.0001). In conclusion, a substantial proportion of diabetes patients in a tertiary care centre presented with an “ambiguous” diabetes type. Their clinical characteristics fall in between those of definite T1DM or T2DM patients.
- Technology/Device
- Glutamic Acid Decarboxylase Autoantibody Detection by Electrochemiluminescence Assay Identifies Latent Autoimmune Diabetes in Adults with Poor Islet Function
- Yuxiao Zhu, Li Qian, Qing Liu, Jing Zou, Ying Zhou, Tao Yang, Gan Huang, Zhiguang Zhou, Yu Liu
- Diabetes Metab J. 2020;44(2):260-266. Published online November 12, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0007
- 5,320 View
- 128 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The detection of glutamic acid decarboxylase 65 (GAD65) autoantibodies is essential for the prediction and diagnosis of latent autoimmune diabetes in adults (LADA). The aim of the current study was to compare a newly developed electrochemiluminescence (ECL)-GAD65 antibody assay with the established radiobinding assay, and to explore whether the new assay could be used to define LADA more precisely.
Methods Serum samples were harvested from 141 patients with LADA, 95 with type 1 diabetes mellitus, and 99 with type 2 diabetes mellitus, and tested for GAD65 autoantibodies using both the radiobinding assay and ECL assay. A glutamic acid decarboxylase antibodies (GADA) competition assay was also performed to assess antibody affinity. Furthermore, the clinical features of these patients were compared.
Results Eighty-eight out of 141 serum samples (62.4%) from LADA patients were GAD65 antibody-positive by ECL assay. Compared with ECL-GAD65 antibody-negative patients, ECL-GAD65 antibody-positive patients were leaner (
P <0.0001), had poorer β-cell function (P <0.05), and were more likely to have other diabetes-associated autoantibodies. The β-cell function of ECL-GAD65 antibody-positive patients was similar to that of type 1 diabetes mellitus patients, whereas ECL-GAD65 antibody-negative patients were more similar to type 2 diabetes mellitus patients.Conclusion Patients with ECL-GAD65 antibody-negative share a similar phenotype with type 2 diabetes mellitus patients, whereas patients with ECL-GAD65 antibody-positive resemble those with type 1 diabetes mellitus. Thus, the detection of GADA using ECL may help to identify the subtype of LADA.
-
Citations
Citations to this article as recorded by- 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Laya Ekhlaspour, Jason L. Gaglia, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Mary Lou Perry, Scott J. Pil
Diabetes Care.2024; 47(Supplement): S20. CrossRef - 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes—2023
Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer, Billy S. Collins, Jason L. Gaglia, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary
Diabetes Care.2023; 46(Supplement): S19. CrossRef - Determination of autoantibodies in type 2 diabetes: one simple way to improve classification
Johnny Ludvigsson
Diabetologia.2023; 66(5): 955. CrossRef - 2. Classification and Diagnosis of Diabetes:Standards of Medical Care in Diabetes—2022
Diabetes Care.2022; 45(Supplement): S17. CrossRef - Screening Strategy for Islet Autoantibodies in Diabetes Patients of Different Ages
Xixi Nan, Xia Li, Yufei Xiang, Xiang Yan, Houde Zhou, Xiaohan Tang, Jin Cheng, Xiaohong Niu, Jing Liu, Qiuhe Ji, Linong Ji, Gan Huang, Zhiguang Zhou
Diabetes Technology & Therapeutics.2022; 24(3): 212. CrossRef - Atypical Diabetes and Management Considerations
Shivajirao Prakash Patil
Primary Care: Clinics in Office Practice.2022; 49(2): 225. CrossRef - Latent autoimmune diabetes in adults: a focus on β-cell protection and therapy
Wenfeng Yin, Shuoming Luo, Zilin Xiao, Ziwei Zhang, Bingwen Liu, Zhiguang Zhou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Analysis of detrended fluctuation function derived from continuous glucose monitoring may assist in distinguishing latent autoimmune diabetes in adults from T2DM
Liyin Zhang, Qi Tian, Keyu Guo, Jieru Wu, Jianan Ye, Zhiyi Ding, Qin Zhou, Gan Huang, Xia Li, Zhiguang Zhou, Lin Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Prevalence of antibodies targeting ubiquitin-conjugating enzyme 2L3 and eukaryote translation elongation factor 1 α1 in Chinese Han and American Caucasian populations with type 1 diabetes
Li Qian, Yuxiao Zhu, Yan Luo, Mu Zhang, Liping Yu, Yu Liu, Tao Yang
Endocrine Connections.2022;[Epub] CrossRef - 2. Classification and Diagnosis of Diabetes:Standards of Medical Care in Diabetes—2021
Diabetes Care.2021; 44(Supplement): S15. CrossRef - High-Affinity ZnT8 Autoantibodies by Electrochemiluminescence Assay Improve Risk Prediction for Type 1 Diabetes
Xiaofan Jia, Ling He, Dongmei Miao, Kathleen Waugh, Cristy Geno Rasmussen, Fran Dong, Andrea K Steck, Marian Rewers, Liping Yu
The Journal of Clinical Endocrinology & Metabolism.2021;[Epub] CrossRef - Lada or Type 2 Diabetes Mellitus - A Challenging Diagnosis in Clinical Approach
Lucia Mihaela Custură, Oana Deteşan, Raluca Maria Tilinca, Reka Annamaria Schmiedt, Brigitta Irén Bacso, Mariana Cornelia Tilinca
Acta Medica Transilvanica.2021; 26(3): 55. CrossRef - A fluorescence enhancement assay for measurement of glutamate decarboxylase activity
Messripour Manoochehr, Mesripour Azadeh
Open Journal of Analytical and Bioanalytical Chemistry.2020; : 007. CrossRef
- 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024
- Correlations between Glucagon Stimulated C-peptide Levels and Microvascular Complications in Type 2 Diabetes Patients
- Hye-Jin Yoon, Youn-Zoo Cho, Ji-young Kim, Byung-Joon Kim, Keun-Young Park, Gwan-Pyo Koh, Dae-Ho Lee, Dong-Mee Lim
- Diabetes Metab J. 2012;36(5):379-387. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.379
- 5,922 View
- 43 Download
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study aimed to investigate whether stimulated C-peptide is associated with microvascular complications in type 2 diabetes mellitus (DM).
Methods A cross-sectional study was conducted in 192 type 2 diabetic patients. Plasma basal C-peptide and stimulated C-peptide were measured before and 6 minutes after intravenous injection of 1 mg glucagon. The relationship between C-peptide and microvascular complications was statistically analyzed.
Results In patients with retinopathy, basal C-peptide was 1.9±1.2 ng/mL, and stimulated C-peptide was 2.7±1.6 ng/mL; values were significantly lower compared with patients without retinopathy (
P =0.031 andP =0.002, respectively). In patients with nephropathy, basal C-peptide was 1.6±0.9 ng/mL, and stimulated C-peptide was 2.8±1.6 ng/mL; values were significantly lower than those recorded in patients without nephropathy (P =0.020 andP =0.026, respectively). Stimulated C-peptide level was associated with increased prevalence of microvascular complications. Age-, DM duration-, and hemoglobin A1c-adjusted odds ratios for retinopathy in stimulated C-peptide value were 4.18 (95% confidence interval [CI], 1.40 to 12.51) and 3.35 (95% CI, 1.09 to 10.25), respectively. The multiple regression analysis between nephropathy and C-peptide showed that stimulated C-peptide was statistically correlated with nephropathy (P =0.03).Conclusion In patients with type 2 diabetes, the glucagon stimulation test was a relatively simple method of short duration for stimulating C-peptide response. Stimulated C-peptide values were associated with microvascular complications to a greater extent than basal C-peptides.
-
Citations
Citations to this article as recorded by- A Nomogram for Predicting Vision-Threatening Diabetic Retinopathy Among Mild Diabetic Retinopathy Patients: A Case–Control and Prospective Study of Type 2 Diabetes
Jing Ke, Kun Li, Bin Cao
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 275. CrossRef - The average 30-minute post-prandial C-peptide predicted diabetic retinopathy progress: a retro-prospective study
Ting Pan, Jie Gao, Xinghua Cai, Huihui Zhang, Jun Lu, Tao Lei
BMC Endocrine Disorders.2023;[Epub] CrossRef - Dysregulation of miR-374a is involved in the progression of diabetic retinopathy and regulates the proliferation and migration of retinal microvascular endothelial cells
Zhanhong Wang, Xiao Zhang, Yanjun Wang, Dailing Xiao
Clinical and Experimental Optometry.2022; 105(3): 287. CrossRef - The Relationship between the Lipid Accumulation Product and Beta-cell Function in Korean Adults with or without Type 2 Diabetes Mellitus: The 2015 Korea National Health and Nutrition Examination Survey
Hye Eun Cho, Seung Bum Yang, Mi Young Gi, Ju Ae Cha, so Young Park, Hyun Yoon
Endocrine Research.2022; 47(2): 80. CrossRef - Effects of Serum C-Peptide Level on Blood Lipid and Cardiovascular and Cerebrovascular Injury in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis
Juan Qin, Rongli Sun, Ding Ding, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022; 2022: 1. CrossRef - Investigation of Diabetes Complication Risk Perception and Diabetes Self-Management Skills in Individuals with Diabetes
Mehmet AYTEMUR, Bahar İNKAYA
Turkish Journal of Diabetes and Obesity.2022; 6(2): 121. CrossRef - Diabetic Retinopathy and Insulin Insufficiency: Beta Cell Replacement as a Strategy to Prevent Blindness
Eli Ipp
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of C-peptide with diabetic vascular complications in type 2 diabetes
Y. Wang, H. Wan, Y. Chen, F. Xia, W. Zhang, C. Wang, S. Fang, K. Zhang, Q. Li, N. Wang, Y. Lu
Diabetes & Metabolism.2020; 46(1): 33. CrossRef - Variations in glucose/C-peptide ratio in patients with type 2 diabetes associated with renal function
John A. D'Elia, Christopher Mulla, Jiankang Liu, Larry A. Weinrauch
Diabetes Research and Clinical Practice.2019; 150: 1. CrossRef - The pharmacokinetics of porcine C‐peptide after intraperitoneal injection
Naho Iizuka, Masuhiro Nishimura, Yasutaka Fujita, Osamu Sawamoto, Shinichi Matsumoto
Xenotransplantation.2019;[Epub] CrossRef - Association of KCNJ11(RS5219) gene polymorphism with biochemical markers of glycemic status and insulin resistance in gestational diabetes mellitus
Lenin M, Ramesh Ramasamy, Sweta Kulkarani, Seetesh Ghose, Srinivasan A.R.S., Sathish Babu M
Meta Gene.2018; 16: 134. CrossRef - Glucagon secretion is increased in patients with Type 2 diabetic nephropathy
Xiaoyu Wang, Juhong Yang, Baocheng Chang, Chunyan Shan, Yanguang Xu, Miaoyan Zheng, Ying Wang, Huizhu Ren, Liming Chen
Journal of Diabetes and its Complications.2016; 30(3): 488. CrossRef - Relationship between serum C-peptide level and diabetic retinopathy according to estimated glomerular filtration rate in patients with type 2 diabetes
Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
Journal of Diabetes and its Complications.2015; 29(3): 350. CrossRef - Independent association between serum C‐peptide levels and fat mass‐to‐lean mass ratio in the aging process
Ying Li, Lian Shun Zheng, Yue Li, Duo Duo Zhao, Lu Meng
Geriatrics & Gerontology International.2015; 15(7): 918. CrossRef - Relationship Between β-Cell Function, Metabolic Control, and Microvascular Complications in Type 2 Diabetes Mellitus
Lihua Zhao, Jing Ma, Shaoxin Wang, Yun Xie
Diabetes Technology & Therapeutics.2015; 17(1): 29. CrossRef - Association of fasting insulin and C peptide with diabetic retinopathy in Latinos with type 2 diabetes
Jane Z Kuo, Xiuqing Guo, Ronald Klein, Barbara E Klein, Robert N Weinreb, Pauline Genter, Fone-Ching Hsiao, Mark O Goodarzi, Jerome I Rotter, Yii-Der Ida Chen, Eli Ipp
BMJ Open Diabetes Research & Care.2014; 2(1): e000027. CrossRef - Association between physical activity and serum C‐peptide levels among the elderly
Ying Li, Lu Meng, QianQian Miao, Yasuto Sato
Geriatrics & Gerontology International.2014; 14(3): 647. CrossRef - Age at Diagnosis and C-Peptide Level Are Associated with Diabetic Retinopathy in Chinese
Xiaoling Cai, Xueyao Han, Simin Zhang, Yingying Luo, Yingli Chen, Linong Ji, Alfred S. Lewin
PLoS ONE.2014; 9(3): e91174. CrossRef - Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset Type 1 and Type 2 Diabetes
Ramachandran Rajalakshmi, Anandakumar Amutha, Harish Ranjani, Mohammed K. Ali, Ranjit Unnikrishnan, Ranjit Mohan Anjana, K.M. Venkat Narayan, Viswanathan Mohan
Journal of Diabetes and its Complications.2014; 28(3): 291. CrossRef - Prediction of response to GLP-1 receptor agonist therapy in Japanese patients with type 2 diabetes
Kenjiro Imai, Tetsuro Tsujimoto, Atsushi Goto, Maki Goto, Miyako Kishimoto, Ritsuko Yamamoto-Honda, Hiroshi Noto, Hiroshi Kajio, Mitsuhiko Noda
Diabetology & Metabolic Syndrome.2014;[Epub] CrossRef - The Association between the Serum C-Peptide Level and Bone Mineral Density
Ying Li, Hua Liu, Yasuto Sato, Bin He
PLoS ONE.2013; 8(12): e83107. CrossRef - C-Peptide and Its Career from Innocent Bystander to Active Player in Diabetic Atherogenesis
Corinna Lebherz, Nikolaus Marx
Current Atherosclerosis Reports.2013;[Epub] CrossRef - C-Peptide and Vascular Complications in Type 2 Diabetic Subjects
Seok Man Son
Diabetes & Metabolism Journal.2012; 36(5): 345. CrossRef
- A Nomogram for Predicting Vision-Threatening Diabetic Retinopathy Among Mild Diabetic Retinopathy Patients: A Case–Control and Prospective Study of Type 2 Diabetes
- Challenges in Diagnosing Type 1 Diabetes in Different Populations
- Marian Rewers
- Diabetes Metab J. 2012;36(2):90-97. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.90
- 3,967 View
- 48 Download
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes affects today an estimated 366 million people world-wide, including 20 million to 40 million of patients with type 1 diabetes (T1D). While T1D accounts for 5% to 20% of those with diabetes, it is associated with higher morbidity, mortality and health care cost than the more prevalent type 2 diabetes. Patients with T1D require exogenous insulin for survival and should be identified as soon as possible after diagnosis to avoid high morbidity due to a delay in insulin treatment. It is also important to present to the patient correct prognosis that differs by the type of diabetes. From the research point of view, correct classification should help to identify the etiologies and to develop specific prevention for T1D. This review summarizes evidence that may be helpful in diagnosing T1D in various ethnic groups. Challenges in interpretation of results commonly used to determine the type of diabetes are highlighted.
-
Citations
Citations to this article as recorded by- Evaluation of Corneal Endothelium and Central Corneal Thickness in Children and Adolescents with Type 1 Diabetes
Semra Tiryaki Demir, Ahmet Uçar, Gizem Kara Elitok, Sümeyra Keleş Yeşiltaş, Emine Betül Akbaş Özyürek, Saniye Üke Uzun
Hamidiye Medical Journal.2023; 4(1): 50. CrossRef - Analysis of Corneal and Lens Densitometry Changes in Patients With Type 1 Diabetes Mellitus
Yusuf Cem Yilmaz, Serife Ciloglu Hayat, Sefik Can Ipek
American Journal of Ophthalmology.2023; 254: 23. CrossRef - Altered Prevalence of Pulp Diagnoses in Diabetes Mellitus Patients: A Retrospective Study
Yandy Gonzalez Marrero, Yoshifumi Kobayashi, Mohammad Saqib Ihsan, Lisa A. Pilch, Liyaa Chen, Shuying Jiang, Yi Ye, Daniel H. Fine, Carla Y. Falcon, Paul A. Falcon, Craig S. Hirschberg, Emi Shimizu
Journal of Endodontics.2022; 48(2): 208. CrossRef - The relationship between GAD65 autoantibody and the risk of T1DM onset
Elham Keshavarzi, Behnoud Baradaran Noveiry, Nima Rezaei
Journal of Diabetes & Metabolic Disorders.2022; 21(2): 1935. CrossRef - Ketosis-Prone Type 2 Diabetes (Flatbush Diabetes) in Remission: A Report of Two Cases
Beisi Ji, SumathaChannapatna Suresh, Klynt Bally, Kamrun Naher, Mary A Banerji
Cureus.2022;[Epub] CrossRef - Analysis of immune cell components and immune-related gene expression profiles in peripheral blood of patients with type 1 diabetes mellitus
Jian Lin, Yuanhua Lu, Bizhou Wang, Ping Jiao, Jie Ma
Journal of Translational Medicine.2021;[Epub] CrossRef - Identification of a subgroup of black South Africans with type 1 diabetes who are older at diagnosis but have lower levels of glutamic acid decarboxylase and islet antigen 2 autoantibodies
C. J. Padoa, P. Rheeder, F. J. Pirie, A. A. Motala, J. C. van Dyk, N. J. Crowther
Diabetic Medicine.2020; 37(12): 2067. CrossRef - Evaluation of retinal neurovascular structures by optical coherence tomography and optical coherence tomography angiography in children and adolescents with type 1 diabetes mellitus without clinical sign of diabetic retinopathy
Semra Tiryaki Demir, Ahmet Ucar, Gizem Kara Elitok, Mehmet Egemen Karatas, Murat Karapapak, Oguz Kaan Kutucu, Saniye Uke Uzun, Dilek Guven
Graefe's Archive for Clinical and Experimental Ophthalmology.2020; 258(11): 2363. CrossRef - A Genome-Wide Analysis of Long Noncoding RNAs in Circulating Leukocytes and Their Differential Expression in Type 1 Diabetes Patients
Yihan Liu, Xiaoming Du, Jia Cui, Changlong Li, Meng Guo, Jianyi Lv, Xin Liu, Jingtao Dou, Xiaoyan Du, Hongjuan Fang, Zhenwen Chen, Bernd Stratmann
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Uncommon Presentations of Diabetes: Zebras in the Herd
Karen L. Shidler, Lisa R. Letourneau, Lucia M. Novak
Clinical Diabetes.2020; 38(1): 78. CrossRef - Changes in Retinal Microcirculation Precede the Clinical Onset of Diabetic Retinopathy in Children With Type 1 Diabetes Mellitus
Merve Inanc, Kemal Tekin, Hasan Kiziltoprak, Servan Ozalkak, Sibel Doguizi, Zehra Aycan
American Journal of Ophthalmology.2019; 207: 37. CrossRef - Autoimmune signatures for prediction and diagnosis of autoimmune diabetes in Kuwait
Mohamed Jahromi, Fahd Al-Mulla, Ebaa Al-Ozairi
Autoimmunity Reviews.2019; 18(6): 642. CrossRef - Human Leukocyte Antigen (HLA) and Islet Autoantibodies Are Tools to Characterize Type 1 Diabetes in Arab Countries: Emphasis on Kuwait
Mohamed Jahromi, Ebaa Al-Ozairi
Disease Markers.2019; 2019: 1. CrossRef - Complete loss of insulin secretion capacity in type 1A diabetes patients during long‐term follow up
Sae Uno, Akihisa Imagawa, Junji Kozawa, Kenji Fukui, Hiromi Iwahashi, Iichiro Shimomura
Journal of Diabetes Investigation.2018; 9(4): 806. CrossRef - Incidence of type 1 diabetes has doubled in Kuwaiti children 0-14 years over the last 20 years
Azza A. Shaltout, Deborah Wake, Thangavel A. Thanaraj, Dina M. Omar, Dalia Al-AbdulRazzaq, Arshad Channanath, Hessa AlKandari, Majedah Abdulrasoul, Sophie Miller, Nicholas Conway, Jaakko Tuomilehto, Lena Davidsson
Pediatric Diabetes.2017; 18(8): 761. CrossRef - Objective Evaluation of Corneal and Lens Clarity in Children With Type 1 Diabetes Mellitus
Kemal Tekin, Merve Inanc, Erdal Kurnaz, Elvan Bayramoglu, Emre Aydemir, Mustafa Koc, Zehra Aycan
American Journal of Ophthalmology.2017; 179: 190. CrossRef - Differential association of body mass index on glycemic control in type 1 diabetes
Eun Young Lee, Yong‐ho Lee, Sang‐Man Jin, Hae Kyung Yang, Chang Hee Jung, Cheol‐Young Park, Jae Hyoung Cho, Woo Je Lee, Byung‐Wan Lee, Jae Hyeon Kim
Diabetes/Metabolism Research and Reviews.2017;[Epub] CrossRef - Progress and challenges in macroencapsulation approaches for type 1 diabetes (T1D) treatment: Cells, biomaterials, and devices
Shang Song, Shuvo Roy
Biotechnology and Bioengineering.2016; 113(7): 1381. CrossRef - Covariation of the Incidence of Type 1 Diabetes with Country Characteristics Available in Public Databases
Paula Andrea Diaz-Valencia, Pierre Bougnères, Alain-Jacques Valleron
PLOS ONE.2015; 10(2): e0118298. CrossRef - Glycated albumin and the risk of micro- and macrovascular complications in subjects with Type 1 Diabetes
Hye-jin Yoon, Yong-ho Lee, So Ra Kim, Tyler Hyungtaek Rim, Eun Young Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Cardiovascular Diabetology.2015;[Epub] CrossRef - Lipid peroxidation and antioxidant protection in girls with type 1 diabetes mellitus during reproductive system development
Lubov I. Kolesnikova, Marina A. Darenskaya, Natalia V. Semenova, Lyudmila A. Grebenkina, Larisa V. Suturina, Marya I. Dolgikh, Svetlana V. Gnusina
Medicina.2015; 51(2): 107. CrossRef - Diagnostic criteria for acute‐onset type 1 diabetes mellitus (2012): Report of the Committee of Japan Diabetes Society on the Research of Fulminant and Acute‐onset Type 1 Diabetes Mellitus
Eiji Kawasaki, Taro Maruyama, Akihisa Imagawa, Takuya Awata, Hiroshi Ikegami, Yasuko Uchigata, Haruhiko Osawa, Yumiko Kawabata, Tetsuro Kobayashi, Akira Shimada, Ikki Shimizu, Kazuma Takahashi, Masao Nagata, Hideichi Makino, Toshiaki Hanafusa
Journal of Diabetes Investigation.2014; 5(1): 115. CrossRef - The Glycated Albumin to Glycated Hemoglobin Ratio Might Not Be Associated with Carotid Atherosclerosis in Patients with Type 1 Diabetes
Wonjin Kim, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Diabetes & Metabolism Journal.2014; 38(6): 456. CrossRef - Diabetes mellitus associada à desnutrição proteica: realidade ou ficção?
Ana Rita Caldas, André Couto Carvalho, Anabela Giestas, Marta Almeida Ferreira, Cláudia Amaral, Cláudia Freitas, Maria Helena Cardoso
Revista Portuguesa de Endocrinologia, Diabetes e Metabolismo.2014; 9(1): 79. CrossRef - Diagnostic criteria for acute-onset type 1 diabetes mellitus (2012)
Eiji Kawasaki, Taro Maruyama, Akihisa Imagawa, Takuya Awata, Hiroshi Ikegami, Yasuko Uchigata, Haruhiko Osawa, Yumiko Kawabata, Tetsuro Kobayashi, Akira Shimada, Ikki Shimizu, Kazuma Takahashi, Masao Nagata, Hideichi Makino, Toshiaki Hanafusa
Diabetology International.2013; 4(4): 221. CrossRef - Phenylmethimazole Suppresses dsRNA-Induced Cytotoxicity and Inflammatory Cytokines in Murine Pancreatic Beta Cells and Blocks Viral Acceleration of Type 1 Diabetes in NOD Mice
Kelly McCall, Martin Schmerr, Jean Thuma, Calvin James, Maria Courreges, Fabian Benencia, Ramiro Malgor, Frank Schwartz
Molecules.2013; 18(4): 3841. CrossRef - Variation of C peptide decay rate in diabetic patients with positive glutamic acid decarboxylase antibody: better discrimination with initial fasting C peptide
Xia Li, Gan Huang, Jian Lin, Lin Yang, Zhiguang Zhou
BMC Endocrine Disorders.2013;[Epub] CrossRef - The Emerging Global Epidemic of Type 1 Diabetes
Jaakko Tuomilehto
Current Diabetes Reports.2013; 13(6): 795. CrossRef - Clinical characteristics and insulin independence of Koreans with new‐onset type 2 diabetes presenting with diabetic ketoacidosis
H. Seok, C. H. Jung, S. W. Kim, M. J. Lee, W. J. Lee, J. H. Kim, B‐W. Lee
Diabetes/Metabolism Research and Reviews.2013; 29(6): 507. CrossRef - Diabetes mellitus and inflammatory pulpal and periapical disease: a review
S. M. F. Lima, D. C. Grisi, E. M. Kogawa, O. L. Franco, V. C. Peixoto, J. F. Gonçalves‐Júnior, M. P. Arruda, T. M. B. Rezende
International Endodontic Journal.2013; 46(8): 700. CrossRef - UM OLHAR SOBRE O DIABETES NA INFÂNCIA E NA JUVENTUDE: NEM TODOS SÃO TIPO 1
Mauren Isfer ANGHEBEM-OLIVEIRA
Infarma - Ciências Farmacêuticas.2013; 25(4): 206. CrossRef - Proteome‐base biomarkers in diabetes mellitus: Progress on biofluids' protein profiling using mass spectrometry
Ana Isabel Padrão, Rita Ferreira, Rui Vitorino, Francisco Amado
PROTEOMICS – Clinical Applications.2012; 6(9-10): 447. CrossRef - Diabetes mellitus: formas de presentación clínica y diagnóstico diferencial de la hiperglucemia en la infancia y adolescencia
Ó. Rubio Cabezas, J. Argente
Anales de Pediatría.2012; 77(5): 344.e1. CrossRef
- Evaluation of Corneal Endothelium and Central Corneal Thickness in Children and Adolescents with Type 1 Diabetes
- Factors Associated with Long-Term Oral Hypoglycemic Agent Responsiveness in Korean Patients with Type 2 Diabetes Mellitus
- Bo-Yeon Kim, Chan-Hee Jung, Ji-Oh Mok, Chul-Hee Kim
- Diabetes Metab J. 2011;35(3):282-289. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.282
- 3,361 View
- 28 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study was performed to determine the factors associated with long-term oral hypoglycemic agent (OHA) responsiveness in Korean type 2 diabetic patients.
Methods Two groups of patients were selected among the type 2 diabetic patients who were followed for more than two years at a university hospital diabetes clinic. The OHA responsive group consisted of 197 patients whose HbA1c levels were maintained at ≤7% with OHA for more than two years. The OHA failure group consisted of 180 patients whose HbA1c levels were >8% in spite of optimal combined OHA therapy or patients who required insulin therapy within the two years of the study.
Results The OHA failure group had higher baseline values of fasting and postprandial glucose, HbA1c, and lower fasting, postprandial, and delta C-peptide compared to those of the OHA responsive group. The OHA failure group also had a higher proportion of female patients, longer diabetic duration, and more family history of diabetes. There were no significant differences in body mass index (BMI) or insulin resistance index between the two groups. Multiple logistic regression analysis showed that the highest quartile of baseline fasting, postprandial glucose, and HbA1c and the lowest quartile of postprandial and delta C-peptide were associated with an increased odds ratio of OHA failure after adjustment for age, sex, body mass index, and family history of diabetes.
Conclusion Lower baseline values of postprandial and delta C-peptide and elevated fasting glucose and HbA1c are associated with long-term OHA responsiveness in Korean patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
Sang-Yong Kim, Sungrae Kim
Diabetes Therapy.2023; 14(1): 109. CrossRef - Cyanidin-3-glucoside isolated from mulberry fruits protects pancreatic β-cells against glucotoxicity-induced apoptosis
JONG SEOK LEE, YOUNG RAE KIM, JUN MYOUNG PARK, YOUNG EON KIM, NAM IN BAEK, EOCK KEE HONG
Molecular Medicine Reports.2015; 11(4): 2723. CrossRef - The Duration of Sulfonylurea Treatment Is Associated withβ-Cell Dysfunction in Patients with Type 2 Diabetes Mellitus
Mi-Seon Shin, Jee Hee Yu, Chang Hee Jung, Jenie Yoonoo Hwang, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park
Diabetes Technology & Therapeutics.2012; 14(11): 1033. CrossRef - The ratio of glycated albumin to glycated haemoglobin correlates with insulin secretory function
Daham Kim, Kwang J. Kim, Ji H. Huh, Byung‐Wan Lee, Eun S. Kang, Bong S. Cha, Hyun C. Lee
Clinical Endocrinology.2012; 77(5): 679. CrossRef
- Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
- Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients
- Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
- Diabetes Metab J. 2011;35(1):41-49. Published online February 28, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.1.41
- 4,052 View
- 37 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have revealed that C-peptide induces smooth muscle cell proliferation and causes human atherosclerotic lesions in diabetic patients. The present study was designed to examine whether the basal C-peptide levels correlate with cardiovascular risk in type 2 diabetes mellitus (T2DM) patients.
Methods Data was obtained from 467 patients with T2DM from two institutions who were followed for four years. The medical findings of all patients were reviewed, and patients with creatinine >1.4 mg/dL, any inflammation or infection, hepatitis, or type 1 DM were excluded. The relationships between basal C-peptide and other clinical values were statistically analyzed.
Results A simple correlation was found between basal C-peptide and components of metabolic syndrome (MS). Statistically basal C-peptide levels were significantly higher than the three different MS criteria used in the present study, the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program's (NCEP's), World Health Organization (WHO), and the International Diabetes Federation (IDF) criteria (NCEP-ATP III,
P =0.001; IDF,P <0.001; WHO,P =0.029). The multiple regression analysis between intima-media thickness (IMT) and clinical values showed that basal C-peptide significantly correlated with IMT (P =0.043), while the analysis between the 10-year coronary heart disease risk by the United Kingdom Prospective Diabetes Study risk engine and clinical values showed that basal C-peptide did not correlate with IMT (P =0.226).Conclusion Basal C-peptide is related to cardiovascular predictors (IMT) of T2DM, suggesting that basal C-peptide does provide a further indication of cardiovascular disease.
-
Citations
Citations to this article as recorded by- The Correlation Between C-Peptide and Severity of Peripheral Atherosclerosis in Type 2 Diabetes Mellitus
Maisa A Wahab, Alshaymaa Alhabibi, Ahmed Khairy Sakr, Mohamed Yahia Zakaria, Ola I Saleh, Inass Hassan Ahmad, Eman Abdelrahman, Randa Taha, Fayka Karem Abdel Azeem Ahmed, Bothayna Ismail, Lamiaa Hosney Azel, Asmaa S Hassan, Hanaa Mohammed Eid El Sayed, Sa
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2617. CrossRef - Blood C‐peptide concentration as a proxy marker of cardiovascular disease: An observational cross‐sectional study
Laurinda Adusu‐Donkor, Emmanuel Kwaku Ofori, Fleischer C. N. Kotey, Francis Kwaku Dogodzi, Wormenor Dziedzorm, Alfred Buabeng, Segla Kwame Bernard, Seth K. Amponsah, Henry Asare‐Anane
Health Science Reports.2023;[Epub] CrossRef - The impact of insulin induced lipohypertrophy on carotid intima-media thickness in patients with type 2 diabetes mellitus
Cem Onur Kirac, Vehbi Sirikci, Huseyin Avni Findikli
Medicine.2023; 102(39): e34696. CrossRef - Effects of Serum C-Peptide Level on Blood Lipid and Cardiovascular and Cerebrovascular Injury in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis
Juan Qin, Rongli Sun, Ding Ding, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022; 2022: 1. CrossRef - Correlation between serum C-peptide-releasing effects and the risk of elevated uric acid in type 2 diabetes mellitus
Yanyan Liu, Xue Zhao, Zequn Yang, Shurui Wang, Cong Han, Huijuan Zhang
Endocrine Journal.2022; 69(7): 773. CrossRef - Human C-peptide is a ligand of the elastin-receptor-complex and therewith central to human vascular remodelling and disease in metabolic syndrome
Gert Wensvoort
Medical Hypotheses.2022; 168: 110964. CrossRef - Influence of blood glucose fluctuation, C-peptide level and conventional risk factors on carotid artery intima–media thickness in Chinese Han patients with type 2 diabetes mellitus
Min Liu, Li Ao, Xinyu Hu, Jianning Ma, Kena Bao, Ye Gu, Jing Zhao, Weiping Huang
European Journal of Medical Research.2019;[Epub] CrossRef - Serum C peptide and carotid intima-medial thickness are independent markers of glucose intolerance among patients with ischemic cerebrovascular stroke
Nearmeen M. Rashad, Ghada M. Samir, Hanan M. Sabry, Nesreen M. Mohy, Shereen M. El Shabrawy
The Egyptian Journal of Internal Medicine.2019; 31(3): 368. CrossRef - Biomarker potential of C-peptide for screening of insulin resistance in diabetic and non-diabetic individuals
Haseeb A. Khan, Samia H. Sobki, Aishah Ekhzaimy, Isra Khan, Mona A. Almusawi
Saudi Journal of Biological Sciences.2018; 25(8): 1729. CrossRef - SERUM C-PEPTIDE LEVEL IN OBESE AND NON-OBESE PATIENTS WITH TYPE 2 DIABETES MELLITUS
Shamha Beegum Mariyam, Saboora Beegum Muthubeevi, Sandhya Chandrasekharan Vasantha
Journal of Evolution of Medical and Dental Sciences.2017; 6(05): 350. CrossRef - Mechanisms of action and therapeutic potential of proinsulin C-peptide
A. O. Shpakov
Journal of Evolutionary Biochemistry and Physiology.2017; 53(3): 180. CrossRef - Hemolysis Affects C‐Peptide Immunoassay
Zhi‐Qi Wu, Ju Lu, Hua‐Guo Xu
Journal of Clinical Laboratory Analysis.2016; 30(6): 1232. CrossRef - Lipid and inflammatory biomarker profiles in early insulin resistance
Itahisa Marcelino Rodríguez, José Oliva García, José Juan Alemán Sánchez, Delia Almeida González, Santiago Domínguez Coello, Buenaventura Brito Díaz, Fadoua Gannar, María del Cristo Rodríguez Pérez, Roberto Elosua, Antonio Cabrera de León
Acta Diabetologica.2016; 53(6): 905. CrossRef - C-Peptide Is Independently Associated with an Increased Risk of Coronary Artery Disease in T2DM Subjects: A Cross-Sectional Study
Lingshu Wang, Peng Lin, Aixia Ma, Huizhen Zheng, Kexin Wang, Wenjuan Li, Chuan Wang, Ruxing Zhao, Kai Liang, Fuqiang Liu, Xinguo Hou, Jun Song, Yiran Lu, Ping Zhu, Yu Sun, Li Chen, Marta Letizia Hribal
PLOS ONE.2015; 10(6): e0127112. CrossRef - C-peptide as a risk factor of coronary artery disease in the general population
Antonio Cabrera de León, José Gregorio Oliva García, Itahisa Marcelino Rodríguez, Delia Almeida González, José Juan Alemán Sánchez, Buenaventura Brito Díaz, Santiago Domínguez Coello, Vicente Bertomeu Martínez, Armando Aguirre Jaime, María del Cristo Rodr
Diabetes and Vascular Disease Research.2015; 12(3): 199. CrossRef - Gender differences in the association of insulin resistance and high-sensitivity c-reactive protein in obese adolescents
Ramin Alemzadeh, Jessica Kichler
Journal of Diabetes & Metabolic Disorders.2014;[Epub] CrossRef - Cytokinome Profile of Patients with Type 2 Diabetes and/or Chronic Hepatitis C Infection
Susan Costantini, Francesca Capone, Eliana Guerriero, Raffaele Marfella, Angela Sorice, Patrizia Maio, Michele Di Stasio, Giuseppe Paolisso, Giuseppe Castello, Giovanni Colonna, Patricia Fitzgerald-Bocarsly
PLoS ONE.2012; 7(6): e39486. CrossRef - Serum glycated albumin predicts the progression of carotid arterial atherosclerosis
Sun Ok Song, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Atherosclerosis.2012; 225(2): 450. CrossRef - C-Peptide: A New Mediator of Atherosclerosis in Diabetes
Dusica Vasic, Daniel Walcher
Mediators of Inflammation.2012; 2012: 1. CrossRef - Letter: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetes Patients (Diabetes Metab J 2011;35:41-9)
Min Suk Lee, Hae Jin Kim
Diabetes & Metabolism Journal.2011; 35(2): 188. CrossRef - Response: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients (Diabetes Metab J 2011;35:41-9)
Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
Diabetes & Metabolism Journal.2011; 35(2): 190. CrossRef
- The Correlation Between C-Peptide and Severity of Peripheral Atherosclerosis in Type 2 Diabetes Mellitus
- The Clinical Characteristics of Young Onset Diabetes According to Etiology Based Classification.
- Mina Park, Yang Il Kang, Suk Chon, Seung joon Oh, Jeong taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- Korean Diabetes J. 2006;30(3):190-197. Published online May 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.3.190
- 2,299 View
- 61 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Recently, the number of young diabetic patients is increasing. It is important to understand the characteristics of young diabetes and classify it correctly to manage these patients successfully. We aimed to classify young onset diabetes according to etiology and evaluate the clinical characteristics. METHODS: Young patients (15~30 years old) who have been treated diabetes in Kyunghee medical center in 2004 were included. We investigated family history of diabetes, disease duration, body mass index (BMI), the history of diabetic ketoacidosis, HbA1c, fasting C-peptide, autoantibody, lipid profile and treatment method via medical records. RESULT: Total 85 patients (M:F 40:45) were evaluated. Type 1 diabetes was 45.9%, type 2 diabetes was 23.5% and unclassified group was 25.9%. Many type 2 diabetic patients were overweight or obese (94.8%). Most young diabetic patients were using insulin (95.4%). Many type 1 diabetic patients have been treated by insulin only and many type 2 diabetic patients have been received combined therapy of insulin and oral hypoglycemic agent. The recent HbA1c was average 8.32 +/- 2.7%. The prevalence of diabetic retinopathy, neuropathy and nephropathy was 32.9%, 22.4% and 16.4% as each. CONCLUSION: Nearly half of young onset diabetes was type 1 diabetes but many others were also classified to type 2 diabetes or unclassified group. It is important to provide a consistent algorithm for assessment and investigation for newly diagnosed young diabetic patients. More education and effort are required to control diabetes strictly and prevent its complication. -
Citations
Citations to this article as recorded by- The Difference in Risk Factors Between Adults With Early-Onset (<40 Years Old) Versus Late-Onset (≥40 Years Old) Type 2 Diabetes in a University Hospital From January 2015-December 2017
Marilyn Katrina C Caro, Elaine C Cunanan
Journal of Medicine, University of Santo Tomas.2022; 6(2): 1009. CrossRef - Lifestyle-related predictors affecting prediabetes and diabetes in 20-30-year-old young Korean adults
Kyong Sil Park, Seon Young Hwang
Epidemiology and Health.2020; 42: e2020014. CrossRef - The Clinical Characteristics of the Newly Diagnosed Early Onset (< 40 Years Old) Diabetes in Outpatients' Clinic
Kyung-Soo Kim, Hyun-Ju Oh, Ji-Woon Kim, Yeo-Kyung Lee, Soo-Kyung Kim, Seok-Won Park, Yoo-Lee Kim, Won-Keun Park, Yong-Wook Cho
Korean Diabetes Journal.2010; 34(2): 119. CrossRef - Anti-GAD Antibody in Patients with Adult-Onset Diabetes in Korea
Eun-Gyoung Hong
Korean Diabetes Journal.2009; 33(1): 13. CrossRef
- The Difference in Risk Factors Between Adults With Early-Onset (<40 Years Old) Versus Late-Onset (≥40 Years Old) Type 2 Diabetes in a University Hospital From January 2015-December 2017
- Relationship between C-peptide, Metabolic Control and Chronic Complications in Type 2 Diabetes.
- Jeung Mook Kang, Won Young Lee, Ji Youn Kim, Jung Won Yun, Sun Woo Kim
- Korean Diabetes J. 2002;26(6):490-499. Published online December 1, 2002
- 1,083 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Type 2 diabetes mellitus is a heterogeneous disease characterized by variable degrees of insulin resistance, impaired insulin secretion and increased glucose production. As the decline of beta-cell function in type 2 diabetes is very slow, the relationship between the insulin secretory capacity, the degree of metabolic control and chronic complications is still unclear. The determination of plasma C-peptide allows for the assessment of the endogenous insulin production, even in the presence of exogenous insulin administration. The aim of this study was to evaluate the relationship between the serum C-peptide level and metabolic parameters, and the complications in type 2 diabetes. METHOD: The clinical characteristics and laboratory findings, such as lipid profile, fasting plasma glucose, HbA1C and uric acid, were evaluated, and their relationships with chronic complications analyzed. We measured the serum C-peptide level by radioimmunoassay (RIA) in 384 type 2 diabetes mellitus patients. The patients were divided into quartile groups according to their fasting C-peptide levels (quartile 1: <1.73 ng/mL, n=95; quartile 2:>or=1.73 ng/mL and <2.38 ng/mL, n=95; quartile 3:>or=2.38 ng/mL and <3.18 ng/mL, n=98; quartile 4:>or=3.18 ng/mL, n=96). RESULTS: Patients in the lowest C-peptide quartile showed significantly higher durations of diabetes, HbA1C and postprandial plasma glucose values, and HDL-cholesterol. Conversely, the BMI, systolic blood pressure, total cholesterol and triglyceride were significantly higher in the highest C-peptide quartile. The prevalence of diabetic retinopathy and urinary protein excretion were higher in lowest quartile, and the diastolic blood pressure was highest in the upper quartile, but these were not statistically significant. The associations between C-peptide, and the duration of diabetes, BMI, total cholesterol, triglyceride, HDL cholesterol, postprandial 2 plasma glucose and systolic blood pressure remained significant, even after multiple adjustments. CONCLUSION: In type 2 diabetes, higher C-peptide levels are associated with a component of metabolic syndrome and lower C-peptide levels due to decreased cell reserves, associated with hyperglycemia and microvascular complications
- Peripheral Polyneruopathy and Hypoinsulinemia in Patients with Type 2 Diabetes.
- Y S Jung, K Y Lee, S K Lee, H K Kim, H Y Park, M H Kang
- Korean Diabetes J. 2000;24(2):256-266. Published online January 1, 2001
- 801 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
There is little information on the risk factors for diabetic polyneuro-pathy other than glycemic control and duration of diabetes. The relation between diabetic polyneuropathy and hypoinsulinemia is controversial. This study is to determine whether hypoinsulinemia is an additional factor influencing the development of polyneuropathy in patients with type 2 diabetes. METHODS: We performed an oral glucose tolerance test with C-peptide measure-ment in 1'P2 patients with type 2 diabetes. Peripheral polyneuropathy was diagnosed when the patients had both typical symptoms of polyneuropathy and abnormal physical findings or NCV. We analysed the relation between metabolic variables including fasting and postprandial C-peptide levels and diabetic polyneuropathy. RESULTS: In addition to retinopathy and nephropathy, duration of diabetes, low C-peptide level (fasting and postprandial), insulin use, and high HDL-cholesterol level were associated with diabetic polyneuropathy. Multivariate logistic regression model revealed that an independent assoclation of diabetes duration and postprandial 2-hour C-peptide concentration with polyneuropathy. When we stratified the patients into the two groups according to the median duration of diabetes (8 years), the association of low postprandial C-peptide concentration with polyneuro-pathy was significant only in the shorter duration group(< 8 years). However, significant association of HbA(1c) level was shown in the longar duration group. CONCLUSION: Decreased insulin secretory function of the pancreas as well as increased duration of diabetes was indepandently associated with diabetic polyneuropathy in patients with type 2 diabetes. Hypoinsulinemia might be an additional risk factor for the development of diabetic polyneuropathy in type 2 diabetic patients, particularly with short duration, To confirm these relationship further longitudinal study in a large cohort is necessary.
- Metabolic Factors Influencing Serum Potassium Levels in Diabetic Ketoacidosis.
- Sung Jin Kim, Seung Oh Suh, Sung Hee Ihm, Hyun Kyu Kim, Doo Man Kim, Jae Myung Yoo, Moon Gi Choi, Hyung Joon Yoo
- Korean Diabetes J. 1999;23(5):661-668. Published online January 1, 2001
- 993 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The serum K level is normal or high in the majority of patients with diabetic ketoacidosis (DKA) despite significant total body K+ deficits. This might be due to the combined effects of severe acidosis, insulin deficiency, volume contraction, hyperglycemia and hypertonicity that usually accompany DKA. The aim of this study was to investigate the most likely determinants of the serum K+ levels among metabolic derangements observed in DKA patients. METHODS: The subjects were 88 DKA patients who had normal or high initial serum K+ levels. We anaylzed the correlation between initial serum K' levels and metabolic parameters (arterial pH, arterial HCO(3-) level, anion gap, serum glucose level, osmolality, BUN and fasting C-peptide levels), by simple linear regression analysis and stepwise multiple regression analysis. RESULT: Serum K+ levels correlated significantly with initial arterial pH(r=-0.38, p<0.001), HCO(3-) (r=-0.35, p<0.001), anion gap(r=0.21, p<0.05), serum glucose (r=0.22, p<0.05) and fasting C-peptide (r=-0.33, p<0.05) levels. Among these, arterial HCO(3-), serum glueose and fasting C-peptide levels had significant and independent effects on serum K+ levels. These levels could account for about 33% of the observed variance in serum K+ levels. CONCLUSION: These results suggest that metabolic acidosis and hyperglycemia in DKA, which result primarily from insulin deficit, are the main determinants of increased serum K+ levels.
- Floow-up Study of Clinical and Immunogenetic Chracteristics and Basal C-peptidein Korea Young Age Onset Diabetic Patients.
- Hyun Chul Lee, Duk Hi Kim, Jae Hyun Nam, Chul Woo Ahn, Seong Kil Lim, Kap Bum Huh, Soo Yeon Nam, Seok Won Park, Young Deuk Song, Hyun Soo Kim, Jin Wook Kweon, Kyung Hee Chang, Kyung Rae Kim
- Korean Diabetes J. 1999;23(3):288-298. Published online January 1, 2001
- 1,201 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was undertaken to observe the changes of basal C-peptide level and to compare the clinical and immunogenetic characteristics in newly dignosed young age-onset diabetics in Korea. We studied predictors effecting the change of insulin secretory capacity in these patients. METHODS: 82 newly diagnosed young diabetic patients (mean age; 23.0+7.1, M:F=46:36) were divided into 3 groups according to the initial fasting serum C-peptide level (Classification I, group 1; C-peptide < 0.6 ng/mL, group 2; 0.6 ng/mL C-peptide <1.2 ng/mL, and group 3; 1.2 ng/mL C-peptide) and reclassified by the follow-up (mean follow-up; 3.7 year) fasting serum C-peptide level. RESULTS: According to the initial fasting serum C-peptide level, 17.1% (14/82) of the patients were classified as group 1, 35.4% (29/82) as group 2, and 47.5%(39/82) as group 3. In group 3, body mass index (BMI, p<0.01) and maximal BMI (p<0.01) at onset, family history of diabetes (p=0.01) and stimulated C-peptide increment were significantly higher than those in group 1 and 2. Presence of urine ketone (p<0.01), history of diabetic keto- acidosis (p<0.01), and frequency of insulin therapy at diagnosis (p<0.01) were significantly lower than those in group 1 and 2. No significant differences in onset age, sex, weight loss at onset, HbA1c, anti GAD antibody and HLA-DR were found among the 3 groups. After certain follow-up periods, 37.8% (31/82) of the patients were reclassified as group 1, 24.4% (20/82) as group 2, and 37.8% (31/82) as group 3 according to the follow-up fasting serum C-peptide level(classification II). All of the patients in group 1 in classification I were reclassified as group 1 in classification II. In group 2, 44.8% were reclassified as group 1 and 17.3% were reclassified in group 3. In group 3, 15.4% (6/39) of patients showed a significant decrease in insulin secretory capacity and were reclassified as type I diabetes, and their predictors for decreased insulin secretory capacity were low BMI at onset, low slimulated C-peptide increment, and antiGAD antibody. CONCLUSION: Our study showed that classification of newly diagnosed young diabetics by fasting C-peptide level is not always easy. Therefore follow-up measurement of C-peptide and consideration of clinical characteristics are needed in discriminating the type of diabetes in these groups of diabetics in Korea.
- Disturbance of Cutaneous Microcirculation assessed by Laser Doppler Flowmetry in Non-Insulin Dependent Diabetic patients.
- Jeong Hyun Park, Sang Hee Nam
- Korean Diabetes J. 1997;21(1):56-64. Published online January 1, 2001
- 681 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diabetic microangiopathies are well-known long-term complication of diabetes mellitus, These are wide-spread phenomena, but little is known about the nature of cutaneous microcirculatory disturbance in diabetic patients which could be considered as cutaneous diabetic microangiopathy. To assess the cutaneous microcirculatory disturbance of diabetic patients, we performed this study. METHODS: We performed the laser Doppler flowmetry which has been known to be an accurate device for measuring cutaneous microcirculatory blood flow to 14 control subjects and 16 non-insulin dependent diabetic patients. We used thermal reactive hyperemic technique to the dorsum of right index finger and right great toe for measuring both baseline and maximum cutaneous microcirculatory blood flow. RESULTS: The baseline microcirculatory blood flow measured at 35C did not show any statistically significant differences between control subjects and diabetic patients, on both finger dorsum and toe dorsum. The maximurn microcirculatory blood flow measured at 44C showed statistically significant difference between control subjects and diabetic patients only at toe dorsum, but not at finger dorsum (p<0.05). CONCLUSION: From the above results, we conclude that cutaneous microcirculation is disturbed in noninsulin dependent diabetic patients, which was manifested at the toe dorsum in the condition of maximum blood flow induced by thermal stimulation. Further studies an exact pathophysiology and possible correlations with diabetic microangiopathies, diabetic duration and the level of glycemic control are needed along with more refinement of measurement techniques.
- Significance of Serum Anticardiolipin Antibody in Non-Insulin Dependent Diabetes Mellitus.
- Hee Jin Kim, Young Sun Hong, Yeon Ah Sung, Nan Ho Kyung
- Korean Diabetes J. 1997;21(1):39-48. Published online January 1, 2001
- 859 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The antiphospholipid antibodies have been characteristically found in the patients with autoimmune diseases. Some previous studies revealed that antiphospholipid antibodies are increased in the sera of patients with diabetes and correlate with the extent of neuropathy and measurements of amiphospholipid antibodies may constitute a marker for ongoing damage to nerves. We measured serum anticardiolipin antibodies(IgG, IgM) to assess the prevalence and significance of anticardiolipin antibodies in NIDDM patients. METHOD: Ninety NIDDM patients were screened for lgG/IgM isotypes of anticardiolipin antibodies by enzyme-linked immunosorbent assay and compared with 30 control subjects. RESULTS: 1) The titers and positivities of IgG anticardiolipin antibodies were significantly higher in the sera of NIDDM patients than those of control subjects(P<0.05). 2) In NIDDM patients with IgG anticardiolipin antibody, the titer of serum c-peptide was significantly lower(P<0.05) and the body mass index tended to be lower(P=0.08). 3) There were no significant differences of positivities of IgG anticardiolipin antibodies according to the state of chronic diabetic complications and the mode of treatment(P>0.05). 4) In the patients with NIDDM, no significant association was found between the titers of IgG anticardiolipin antibodies and age, diabetic duration, fasting blood glucose, HbAlc, total cholesterol and triglyceride. CONCLUSION: The titers and positivities of IgG anticardiolipin antibodies were elevated in NIDDM. In the NIDDM patients with IgG anticardiolipin antibody, the serum titers of c-peptide were significantly lower and the body mass index tended to be lower. It seems that serum IgG anticardiolipin antibodies might have autoimmune relationship with slowly progressive IDDM, but further prospective mass studies will be requird.

 KDA
KDA
 First
First Prev
Prev





