
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
- Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
- Min Jeong Park, Kyung Mook Choi
- Diabetes Metab J. 2022;46(1):49-62. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0316
- 5,698 View
- 221 Download
- 5 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 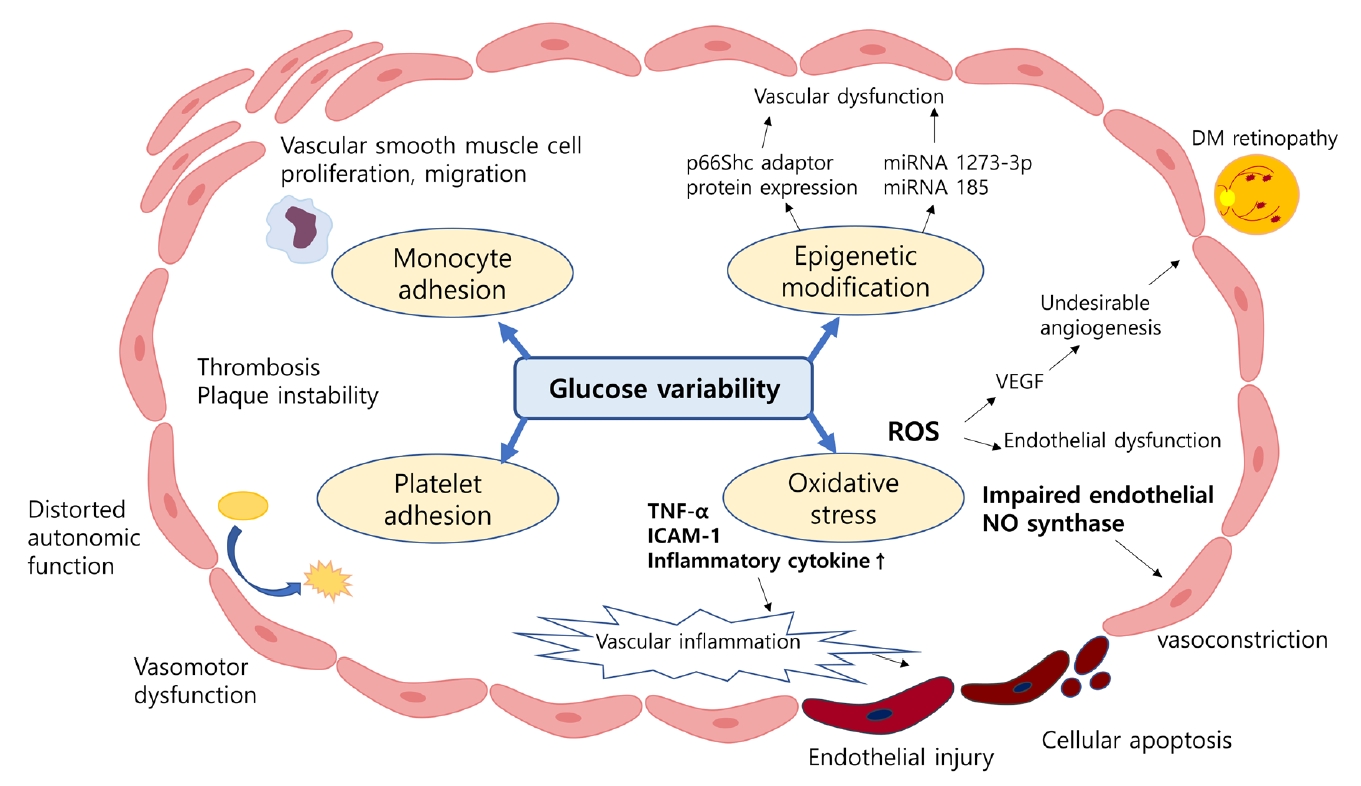
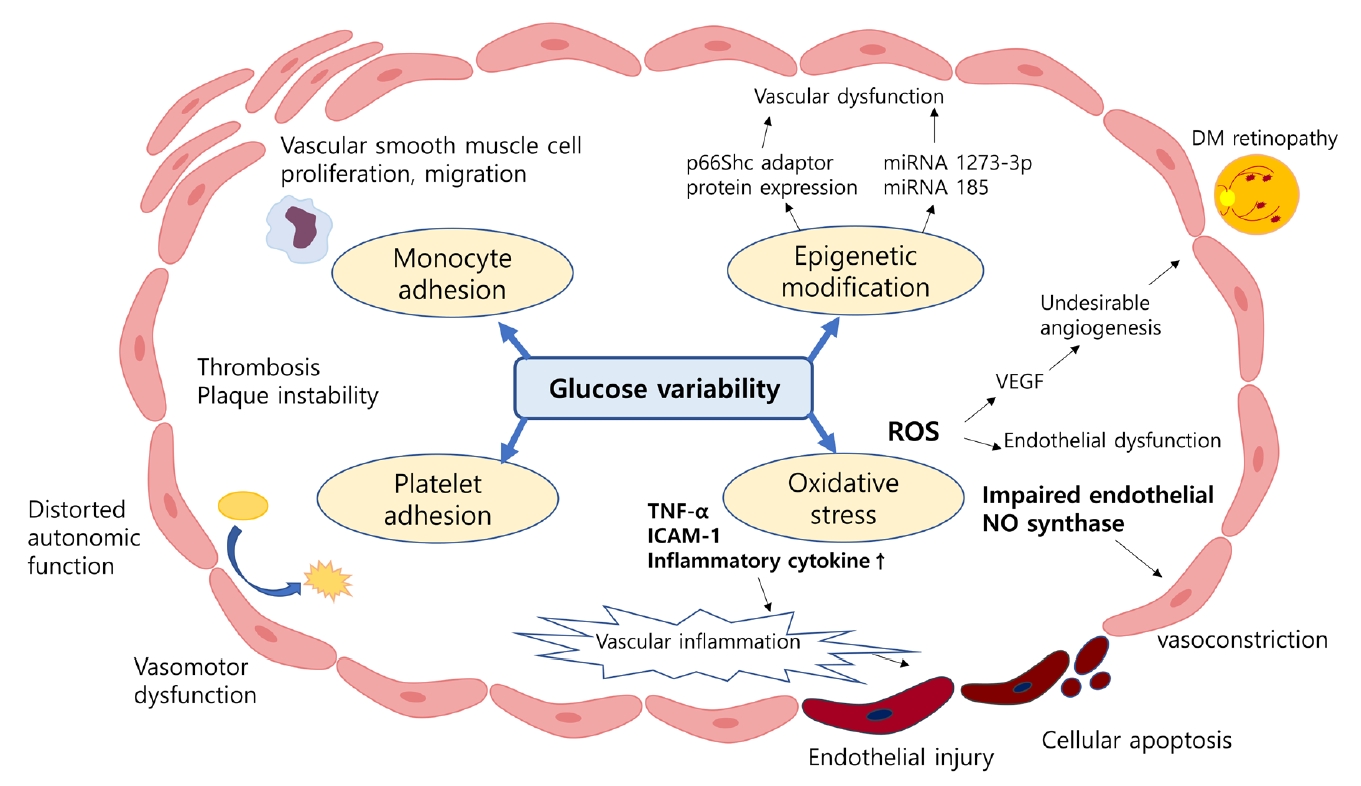
- Despite strenuous efforts to reduce cardiovascular disease (CVD) risk by improving cardiometabolic risk factors, such as glucose and cholesterol levels, and blood pressure, there is still residual risk even in patients reaching treatment targets. Recently, researchers have begun to focus on the variability of metabolic variables to remove residual risks. Several clinical trials and cohort studies have reported a relationship between the variability of metabolic parameters and CVDs. Herein, we review the literature regarding the effect of metabolic factor variability and CVD risk, and describe possible mechanisms and potential treatment perspectives for reducing cardiometabolic risk factor variability.
-
Citations
Citations to this article as recorded by- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
BMC Medicine.2023;[Epub] CrossRef - Dose–response relationship between physical activity and cardiometabolic risk in obese children and adolescents: A pre-post quasi-experimental study
Zekai Chen, Lin Zhu
Frontiers in Physiology.2023;[Epub] CrossRef - Association of body weight change with all-cause and cause-specific mortality: A nationwide population-based study
So Yoon Kwon, Gyuri Kim, Jungkuk Lee, Jiyun Park, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2023; 199: 110666. CrossRef - Association between lipid variability and the risk of mortality in cancer patients not receiving lipid-lowering agents
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Frontiers in Oncology.2023;[Epub] CrossRef - Association between visit-to-visit lipid variability and risk of ischemic heart disease: a cohort study in China
Yonghao Wu, Peng Shen, Lisha Xu, Zongming Yang, Yexiang Sun, Luhua Yu, Zhanghang Zhu, Tiezheng Li, Dan Luo, Hongbo Lin, Liming Shui, Mengling Tang, Mingjuan Jin, Kun Chen, Jianbing Wang
Endocrine.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef - Long-Term Variability in Physiological Measures in Relation to Mortality and Epigenetic Aging: Prospective Studies in the US and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
SSRN Electronic Journal .2022;[Epub] CrossRef
- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
- Clinical Diabetes & Therapeutics
- Effectiveness of Exercise Intervention in Reducing Body Weight and Glycosylated Hemoglobin Levels in Patients with Type 2 Diabetes Mellitus in Korea: A Systematic Review and Meta-Analysis
- Ji-Eun Jang, Yongin Cho, Byung Wan Lee, Ein-Soon Shin, Sun Hee Lee
- Diabetes Metab J. 2019;43(3):302-318. Published online November 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0062
- 5,312 View
- 97 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background This study aimed to assess the effectiveness of exercise intervention in reducing body weight and glycosylated hemoglobin (HbA1c) level in patients with type 2 diabetes mellitus (T2DM) in Korea.
Methods Cochrane, PubMed, Embase, KoreaMed, KMbase, NDSL, KCI, RISS, and DBpia databases were used to search randomized controlled trials and controlled clinical trials that compared exercise with non-exercise intervention among patients with non-insulin-treated T2DM in Korea. The effectiveness of exercise intervention was estimated by the mean difference in body weight changes and HbA1c level. Weighted mean difference (WMD) with its corresponding 95% confidence interval (CI) was used as the effect size. The pooled mean differences of outcomes were calculated using a random-effects model.
Results We identified 7,692 studies through literature search and selected 23 articles (723 participants). Compared with the control group, exercise intervention (17 studies) was associated with a significant decline in HbA1c level (WMD, −0.58%; 95% CI, −0.89 to −0.27;
I 2=73%). Although no significant effectiveness on body weight was observed, eight aerobic training studies showed a significant reduction in body weight (WMD, −2.25 kg; 95% CI, −4.36 to −0.13;I 2=17%) in the subgroup analysis.Conclusion Exercise significantly improves glycemic control; however, it does not significantly reduce body weight. Aerobic training can be beneficial for patients with non-insulin-treated T2DM in Korea.
-
Citations
Citations to this article as recorded by- The anti-inflammatory effects of aerobic exercise training in patients with type 2 diabetes: A systematic review and meta-analysis
Georgia Papagianni, Chrystalla Panayiotou, Michail Vardas, Nikolaos Balaskas, Constantinos Antonopoulos, Dimitrios Tachmatzidis, Triantafyllos Didangelos, Vaia Lambadiari, Nikolaos P.E. Kadoglou
Cytokine.2023; 164: 156157. CrossRef - Glucose Control in Korean Patients with Type 2 Diabetes Mellitus according to Body Mass Index
Ye-lim Shin, Heesoh Yoo, Joo Young Hong, Jooeun Kim, Kyung-do Han, Kyu-Na Lee, Yang-Hyun Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(1): 55. CrossRef - Exercise therapy for diabetes mellitus
Chaiho Jeong, Tae-Seo Sohn
Journal of the Korean Medical Association.2023; 66(7): 427. CrossRef - Effects of an evidence‐based nursing intervention on prevention of anxiety and depression in the postpartum period
Jun Meng, Junying Du, Xiaoli Diao, Yingxia Zou
Stress and Health.2022; 38(3): 435. CrossRef - Effect of exercise intervention dosage on reducing visceral adipose tissue: a systematic review and network meta-analysis of randomized controlled trials
Yu-Hsuan Chang, Hui-Ying Yang, Shiow-Ching Shun
International Journal of Obesity.2021; 45(5): 982. CrossRef - Development and validation of the type 2 diabetes mellitus 10-year risk score prediction models from survey data
Gregor Stiglic, Fei Wang, Aziz Sheikh, Leona Cilar
Primary Care Diabetes.2021; 15(4): 699. CrossRef - Pioglitazone for NAFLD Patients With Prediabetes or Type 2 Diabetes Mellitus: A Meta-Analysis
Jingxuan Lian, Jianfang Fu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Exercise Training: The Holistic Approach in Cardiovascular Prevention
Francesco Giallauria, Teresa Strisciuglio, Gianluigi Cuomo, Anna Di Lorenzo, Andrea D’Angelo, Mario Volpicelli, Raffaele Izzo, Maria Virginia Manzi, Emanuele Barbato, Carmine Morisco
High Blood Pressure & Cardiovascular Prevention.2021; 28(6): 561. CrossRef - Effect of chronic High Intensity Interval Training on glycosylated haemoglobin in people with type 2 diabetes: a meta-analysis
María Cristina Arrieta-Leandro, Jessenia Hernández-Elizondo, Judith Jiménez-Díaz
Human Movement.2021; 24(1): 32. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Factors Influencing Glycemic Control among Type 2 Diabetes Mellitus Patients: The Sixth Korea National Health and Nutrition Examination Survey (2013~2015)
Mee Ock Gu
Korean Journal of Adult Nursing.2019; 31(3): 235. CrossRef
- The anti-inflammatory effects of aerobic exercise training in patients with type 2 diabetes: A systematic review and meta-analysis
- Obesity and Metabolic Syndrome
- Importance of Lean Muscle Maintenance to Improve Insulin Resistance by Body Weight Reduction in Female Patients with Obesity
- Yaeko Fukushima, Satoshi Kurose, Hiromi Shinno, Ha Cao Thu, Nana Takao, Hiromi Tsutsumi, Yutaka Kimura
- Diabetes Metab J. 2016;40(2):147-153. Published online March 27, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.2.147
- 3,585 View
- 48 Download
- 29 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background It has recently been suggested that skeletal muscle has an important role in insulin resistance in obesity, in addition to exercise tolerance and the fat index. The aim of this study was to identify body composition factors that contribute to improvement of insulin resistance in female patients with obesity who reduce body weight.
Methods We studied 92 female obese patients (age 40.9±10.4 years, body mass index 33.2±4.6 kg/m2) who reduced body weight by ≥5% after an intervention program including diet, exercise therapy, and cognitive behavioral therapy. Before and after the intervention, body composition was evaluated by dual-energy X-ray absorptiometry to examine changes in skeletal muscle mass. Homeostasis model assessment of insulin resistance (HOMA-IR) was measured as an index of insulin resistance. Cardiopulmonary exercise was also performed by all patients.
Results There were significant improvements in body weight (–10.3%±4.5%), exercise tolerance (anaerobic threshold oxygen uptake 9.1%±18.4%, peak oxygen uptake 11.0%±14.2%), and HOMA-IR (–20.2%±38.3%). Regarding body composition, there were significant decreases in total body fat (–19.3%±9.6%), total fat-free mass (–2.7%±4.3%), and % body fat (–10.1%±7.5%), whereas % skeletal muscle significantly increased (8.9%±7.2%). In stepwise multiple linear regression analysis with change in HOMA-IR as the dependent variable, the change in % skeletal muscle was identified as an independent predictor (β=–0.280,
R 2=0.068,P <0.01).Conclusion Improvement of insulin resistance in female obese patients requires maintenance of skeletal muscle mass.
-
Citations
Citations to this article as recorded by- Sarcopenia prevalence between obese and morbid obese patients in an obesity center
Mujgan Tuna, Arzu Cennet Işık , Ozlem Hürmeydan
Journal of Surgery and Medicine.2024; 8(4): 73. CrossRef - Dietary behaviour change intervention for managing sarcopenic obesity among community-dwelling older people: a pilot randomised controlled trial
Yue-Heng Yin, Justina Yat Wa Liu, Maritta Välimäki
BMC Geriatrics.2023;[Epub] CrossRef - Diet and Exercise in the Management of Polycystic Ovary Syndrome: Practical Considerations for Person-Centered Care
Giorgia E. Colombo, Stephanie Pirotta, Angelo Sabag
Seminars in Reproductive Medicine.2023; 41(01/02): 026. CrossRef - Effect of Mobility Restrictions During the Coronavirus Disease Epidemic on Body Composition and Exercise Tolerance in Patients With Obesity: Single Institutional Retrospective Cohort Study
Yoshinari Matsumoto, Satoshi Kurose, Takumi Miyauchi, Sawako Yoshiuchi, Daiki Habu, Yutaka Kimura
Journal of Physical Activity and Health.2022; 19(5): 351. CrossRef - Interrelationship of Gut Microbiota, Obesity, Body Composition and Insulin Resistance in Asians with Type 2 Diabetes Mellitus
Che-Sheng Pai, Cheng-Yuan Wang, Wei-Wen Hung, Wei-Chun Hung, Hui-Ju Tsai, Chen-Chia Chang, Shang-Jyh Hwang, Chia-Yen Dai, Wen-Yu Ho, Yi-Chun Tsai
Journal of Personalized Medicine.2022; 12(4): 617. CrossRef - Exercise and Nutrition Strategies for Combating Sarcopenia and Type 2 Diabetes Mellitus in Older Adults
Dionysia Argyropoulou, Nikolaos D. Geladas, Tzortzis Nomikos, Vassilis Paschalis
Journal of Functional Morphology and Kinesiology.2022; 7(2): 48. CrossRef - Branched-Chain and Aromatic Amino Acids in Relation to Fat Mass and Fat-Free Mass Changes among Adolescents: A School-Based Intervention
Magnoudewa Priscille Pana, Pierre Ayotte, Elhadji Anassour-Laouan-Sidi, Edouard Suhas, Clémence Mahana Iti Gatti, Michel Lucas
Metabolites.2022; 12(7): 589. CrossRef - Exercising for Insulin Sensitivity – Is There a Mechanistic Relationship With Quantitative Changes in Skeletal Muscle Mass?
Jasmine Paquin, Jean-Christophe Lagacé, Martin Brochu, Isabelle J. Dionne
Frontiers in Physiology.2021;[Epub] CrossRef - The relationship between changes in serum myostatin and adiponectin levels in patients with obesity undergoing a weight loss program
Nana Takao, Satoshi Kurose, Takumi Miyauchi, Katsuko Onishi, Atsuko Tamanoi, Ryota Tsuyuguchi, Aya Fujii, Sawako Yoshiuchi, Kazuhisa Takahashi, Hiromi Tsutsumi, Yutaka Kimura
BMC Endocrine Disorders.2021;[Epub] CrossRef - Exercise induces favorable metabolic changes in white adipose tissue preventing high‐fat diet obesity
Babu R. Maharjan, Sergio F. Martinez‐Huenchullan, Susan V. Mclennan, Stephen M. Twigg, Paul F. Williams
Physiological Reports.2021;[Epub] CrossRef - THE RELATIONSHIP BETWEEN INSULIN RESISTANCE AND FA-TIGUE SYMPTOM IN FIBROMYALGIA SYNDROME
Türkan Turgay, Zekiye İpek Katirci Kirmaci, Pınar Günel Karadeniz, Mehmet Baştemir
International Journal of Research -GRANTHAALAYAH.2020; 8(3): 271. CrossRef - Epicardial adipose tissue is tightly associated with exercise intolerance in patients with type 2 diabetes mellitus with asymptomatic left ventricular structural and functional abnormalities
Yousuke Sugita, Katsuhiko Ito, Shigeki Sakurai, Satoshi Sakai, Shinya Kuno
Journal of Diabetes and its Complications.2020; 34(5): 107552. CrossRef - Dose Frequency Optimization of the Dual Amylin and Calcitonin Receptor Agonist KBP-088: Long-Lasting Improvement in Food Preference and Body Weight Loss
Anna Thorsø Larsen, Nina Sonne, Kim V. Andreassen, Morten A. Karsdal, Kim Henriksen
Journal of Pharmacology and Experimental Therapeutics.2020; 373(2): 269. CrossRef - Healthy dietary pattern and their corresponding gut microbiota profile are linked to a lower risk of type 2 diabetes, independent of the presence of obesity
D.A. Díaz-Rizzolo, B. Kostov, M. López-Siles, A. Serra, C. Colungo, L. González-de-Paz, M. Martinez-Medina, A. Sisó-Almirall, R. Gomis
Clinical Nutrition.2020; 39(2): 524. CrossRef Changes in Body Composition and FTO Whole Blood DNA Methylation Among Japanese Women: A Randomized Clinical Trial of Weight-Loss Program
Haruhiko Nishida, Katsuko Onishi, Satoshi Kurose, Hiromi Tsutsumi, Takumi Miyauchi, Nana Takao, Sawako Yoshiuchi, Aya Fujii, Yutaka Kimura
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2157. CrossRef- Effects of low skeletal muscle mass and sarcopenic obesity on albuminuria: a 7-year longitudinal study
Jee Hee Yoo, Gyuri Kim, Sung Woon Park, Min Sun Choi, Jiyeon Ahn, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Mira Kang, Jae Hyeon Kim
Scientific Reports.2020;[Epub] CrossRef - Effects of body weight loss program on parameters of muscle performance in female obese adults
Gian Pietro Emerenziani, Dafne Ferrari, Silvia Migliaccio, Andrea Lenzi, Emanuela A. Greco, Chiara Marocco, Carlo Baldari, Laura Guidetti
The Journal of Sports Medicine and Physical Fitness.2019;[Epub] CrossRef - Reduced Lean Body Mass and Cardiometabolic Diseases in Adult Males with Overweight and Obesity: A Pilot Study
Shirine Khazem, Leila Itani, Dima Kreidieh, Dana El Masri, Hana Tannir, Roberto Citarella, Marwan El Ghoch
International Journal of Environmental Research and Public Health.2018; 15(12): 2754. CrossRef - Physical performance measures in screening for reduced lean body mass in adult females with obesity
M. El Ghoch, A.P. Rossi, S. Calugi, S. Rubele, F. Soave, M. Zamboni, E. Chignola, G. Mazzali, P.V. Bazzani, R. Dalle Grave
Nutrition, Metabolism and Cardiovascular Diseases.2018; 28(9): 917. CrossRef - Testosterone a key factor in gender related metabolic syndrome
V. E. Bianchi, V. Locatelli
Obesity Reviews.2018; 19(4): 557. CrossRef - Burly1 is a mouse QTL for lean body mass that maps to a 0.8-Mb region of chromosome 2
Cailu Lin, Brad D. Fesi, Michael Marquis, Natalia P. Bosak, Anna Lysenko, Mohammed Amin Koshnevisan, Fujiko F. Duke, Maria L. Theodorides, Theodore M. Nelson, Amanda H. McDaniel, Mauricio Avigdor, Charles J. Arayata, Lauren Shaw, Alexander A. Bachmanov, D
Mammalian Genome.2018; 29(5-6): 325. CrossRef - Hypoxic Training Improves Normoxic Glucose Tolerance in Adolescents with Obesity
ESTELLE DE GROOTE, FLORIAN A. BRITTO, LOÏC BULLOCK, MARIE FRANÇOIS, CARINE DE BUCK, HENRI NIELENS, LOUISE DELDICQUE
Medicine & Science in Sports & Exercise.2018; 50(11): 2200. CrossRef - Lipid modulation of skeletal muscle mass and function
Christopher Lipina, Harinder S Hundal
Journal of Cachexia, Sarcopenia and Muscle.2017; 8(2): 190. CrossRef - Angiotensin-Converting Enzyme Ins/Del Polymorphism and Body Composition: The Intermediary Role of Hydration Status
Laura Bordoni, Valerio Napolioni, Francesca Marchegiani, Emilio Amadio, Rosita Gabbianelli
Lifestyle Genomics.2017; 10(1-2): 1. CrossRef - Influence of segmental body composition and adiposity hormones on resting metabolic rate and substrate utilization in overweight and obese adults
K. R. Hirsch, A. E. Smith-Ryan, M. N. M. Blue, M. G. Mock, E. T. Trexler
Journal of Endocrinological Investigation.2017; 40(6): 635. CrossRef - Carbohydrate-Restriction with High-Intensity Interval Training: An Optimal Combination for Treating Metabolic Diseases?
Monique E. Francois, Jenna B. Gillen, Jonathan P. Little
Frontiers in Nutrition.2017;[Epub] CrossRef - Mediterranean diet and mortality risk in metabolically healthy obese and metabolically unhealthy obese phenotypes
Y-M Park, S E Steck, T T Fung, J Zhang, L J Hazlett, K Han, A T Merchant
International Journal of Obesity.2016; 40(10): 1541. CrossRef - Effects of Body Weight Reduction on Serum Irisin and Metabolic Parameters in Obese Subjects
Yaeko Fukushima, Satoshi Kurose, Hiromi Shinno, Ha Cao Thi Thu, Nana Takao, Hiromi Tsutsumi, Takaaki Hasegawa, Toshiaki Nakajima, Yutaka Kimura
Diabetes & Metabolism Journal.2016; 40(5): 386. CrossRef
- Sarcopenia prevalence between obese and morbid obese patients in an obesity center
- The percent change of body weight in patients with type 2 diabetes using rosiglitazone for 1 year.
- Seong Bin Hong, Hwi Ra Park, Eun A Kim, Kyung wook Lee, Moonsuk Nam, Yong Seong Kim
- Korean Diabetes J. 2006;30(1):47-53. Published online January 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.1.47
- 1,698 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Rosiglitazone(RSG) is known as a potent agonist for the PPARgamma. It improves glycemic control by improving insulin sensitivity in peripheral tissues. And it is associated with body weight gain. The Pro12Ala polymorphism of the gene encoding the peroxisome proliferator-activated receptor(PPAR)gamma2 has recently been shown to be associated with insulin sensitivity. This study was performed to evaluate the body weight change during the long term rosiglitazone treatment and the role of PPARgamma2 polymorphism, Pro12Ala as an indicator to predict the clinical response of RSG in type 2 diabetes patients. METHOD: The study subjects were 214 type 2 diabetic patients(117 male, 97 female) who were received a daily 1 year course of 4 mg RSG combined with sulfonylurea or metformin. The Pro12Ala polymorphism of the PPARgamma2 was determined by the restriction fragment length polymorphism(RFLP) method. Body weight, height, waist circumference, fasting glucose, insulin, c-peptide and lipid profile were measured. RESULTS: After RSG treatment, body weight change was 2.4 +/- 3.8%, 4.5 +/- 9.8% of baseline body weight at 12, 24 weeks respectively. Body weight gains were increased to 5.6 +/- 10.1% at the end of 1 year. The HbA1C, serum insulin level and HOMA index were decreased following the rosiglitazone therapy. The allele frequency of the Ala12Pro polymorphism of the PPARgamma2 was 0.016. The number of Ala12Pro variant of the PPARgamma2 was too low to predict clinical response of RSG. Body weight gain was correlated with basal fasting plasma glucose, post-prandial 2 hour glucose and HbA1c level(p<0.05). There was no correlation between baseline body weight and change. CONCLUSION: This results showed that Pro12Ala polymorphism was not acceptable for the predictor of RSG induced weight gain and clinical response. However, body weight gain was increased in who had high glucose level, and correlated positively with glucose decrease. 1st 3 month weight gain was best predictor of weight change during 1 year.
- The long term effects of rosiglitazone on serum lipid concentration and body weight.
- Wan Sub Shim, Mi Young Do, Soo Kyung Kim, Hae Jin Kim, Kyu Yeon Hur, Eun Seok Kang, Yu Mie Rhee, Chul Woo Ahn, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2006;30(1):17-24. Published online January 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.1.17
- 2,112 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Although rosiglitazone, an insulin sensitizer, is known to have beneficial effects on high density lipoprotein cholesterol (HDL-C) concentration and low density lipoprotein (LDL) particle size, it has adverse effects on the increment of total cholesterol (TC) and LDL cholesterol (LDL-C), and body weight in some studies. Such adverse effects of rosiglitazone on the serum lipid profiles and body weight seem to be attributed to the fact that most studies with rosiglitazone are limited to a short period of follow up. The aim of this study was to evaluate the long term effects of rosiglitazone on the serum lipid levels and body weight. MATERIALS AND METHODS: We prospectively evaluated fasting serum glucose, HbA1c, TC, LDL-C, triglyceride, HDL-C and body weight at baseline and every three months after rosiglitazone usage (4mg/d) in 202 type 2 diabetic patients. RESULTS: TC levels had increased maximally at 3 months and thereafter decreased, but were significantly higher at 18 months than those at baseline. LDL-C levels from the first 3 months to 12 months were significantly higher than those at baseline, but after 15 months, LDL-C concentration was not significantly different from the basal LDL-C concentration. HDL-C levels had increased after first 3 months and the increment of HDL-C concentration were maintained. The increment of HDL-C was more prominent in patients with low basal HDL-C concentration than in patients with high basal HDL-C concentration. Body weight from 3 months to 18 months were higher than that at baseline, but after 3 months, body weight did not increase furthermore significantly. CONCLUSIONS: The adverse effects on lipid concentration and body weight of rosiglitazone may attenuate after long term usage of rosiglitazone.
- The Role of Chromium as an Insulin Sensitizer in Rats Receivieng Corticosteroid.
- Dong Sun Kim, Chang Beom Lee, Yong Soo Park, You Hern Ahn, Tae Wha Kim, Ho Soon Choi, Il Kyu Park, Hyun Jin Shin, Ju Seop Kang
- Korean Diabetes J. 2001;25(3):211-217. Published online June 1, 2001
- 948 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Chromium (Cr) has been known to be essential for the regulation of insulin action. Recently it has been reported that corticosteroid increases urinary loss of Cr, and that Cr supplementation recovers steroid induced diabetes mellitus. METHODS: Rats were daily treated with dexamethasone (0.2 mg/kg, ip) for first 7 days and were further treated daily with dexamethasone plus either chromium picolinate (30 mg/kg) or a placebo for a period of 14 days. RESULTS: At the end of experiment (Day 21), the control rats treated only with dexamethasone weighed 320 gram (80% of initial weight) in average, but the Cr treated rats weighed 364 gram (91% of initial weight. p<0.05). An insulin sensitivity test [subcutaneous injection of insulin (5 U/kg) plus intraperitoneal injection of glucose (30 minutes after insulin injection)] were conducted. During the insulin sensitivity tests, the area under curves (AUC(0->120 min)) of the time-glucose concentrations curves in the Cr-treated group were decreased compared to those in the control group (5250 vs 15883 mg-min/dL, p<0.01). Fasting serum insulin levels in the Cr-treated rats were clearly decreased by 46.9% compared to those in the control group (2.98 vs 5.60 ng/mL, p<0.05). CONCLUSIONS: We conclude that chromium supplementation reverse a catabolic state, and increase insulin sensitivity in dexamethasone treated rats.

 KDA
KDA
 First
First Prev
Prev





