- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 39(4); 2015 > Article
-
Original ArticleClinical Care/Education Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
- Jin-Hee Jung1,2, Jung-Hwa Lee2,3, Jin-Won Noh4, Jeong-Eun Park2,5, Hee-Sook Kim6, Joo-Wha Yoo2,7, Bok-Rye Song2,8, Jeong-rim Lee2,9, Myeong-Hee Hong2,10, Hyang-Mi Jang2,11, Young Na2,12, Hyun-Joo Lee2,13, Jeong-Mi Lee2,14, Yang-Gyo Kang2,15, Sun-Young Kim2,16, Kang-Hee Sim2,16
-
Diabetes & Metabolism Journal 2015;39(4):307-315.
DOI: https://doi.org/10.4093/dmj.2015.39.4.307
Published online: August 17, 2015
1Division of Diabetes Education Team, Department of Nursing, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
2Korea Association of Diabetes Nurse Educators, Seoul, Korea.
3Division of Diabetes Education Team, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
4Department of Healthcare Management and Institute of Global Healthcare Research, Eulji University School of Medicine, Seongnam, Korea.
5Division of Diabetes Education Team, Cheil General Hospital & Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
6Department of Nursing, Dongnam Health University, Suwon, Korea.
7Division of Diabetes Education Team, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
8Division of Diabetes Education Team , Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
9Division of Diabetes Education Team, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
10Division of Diabetes Education Team, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
11Division of Diabetes Education Team, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
12Division of Diabetes Education Team, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
13Division of Diabetes Education Team, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
14Division of Diabetes Education Team, Kwangmyung Sungae Hospital, Gwangmyeong, Korea.
15Division of Diabetes Education Team, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea.
16Diabetes Education Unit, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding author: Kang-Hee Sim. Diabetes Education Unit, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 06351, Korea. jsmercy@naver.com
- *Jin-Hee Jung and Jung-Hwa Lee contributed equally to this study as first authors
Copyright © 2015 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- In Korea, the prevalence, complications, and mortality rate of diabetes are rapidly increasing. However, investigations on the actual condition of diabetes management are very limited due to lack of nation-wide research or multicenter study. Hence, we have minutely inquired the current status of diabetes management and achievement of glucose target goal in general hospital offering education program. That way, we are able to furnish data for policy making of diabetes education and draw up guideline which may allow us to reduce the morbidity and mortality of diabetes.
-
Methods
- The subjects consisted of 2,610 patients with type 2 diabetes who visited the 13 general hospital in Seoul or Gyeonggi region from March 19 to May 29, 2013. General characteristics, associated diseases, complications, and management status were investigated.
-
Results
- The mean age was 61.0±11.6 years, body mass index was 25.0±3.3 kg/m2, and family history of diabetes was 50.5%. The mean duration of diabetes was 10.7±7.9 years and 53% received education about diabetes. The prevalence of hypertension and dyslipidemia were 59.2% and 65.5%, respectively, and 18.3% of the subjects were accompanied by liver disease. Diabetic retinopathy appeared in 31.6%, nephropathy in 28.1%, and neuropathy in 19.9% of the subjects. The mean glycosylated hemoglobin (HbA1c) level was 7.3%±1.3% and the achieving rate based on Korean Diabetes Association guideline (HbA1c <6.5%) was 24.8%, blood pressure (130/80 mm Hg or less) was 49.4%, and low density lipoprotein cholesterol (<100 mg/dL) was 63.6%. The reaching rate to the target level in four parameters (blood glucose, blood pressure, lipids, and body weight) was 7.8%.
-
Conclusion
- The blood glucose control rate was lower than other parameters, and the implementation rate of diabetes education was only 53%. Thus more appropriate glucose control and systematic diabetes education are imperative.
- Diabetes mellitus is a chronic disease whose prevalence is rapidly increasing worldwide, with the number of diabetic patients being expected to increase from 360 million in 2011 to 550 million by 2030 [1]. This increase is especially faster in Asia including China, India, and Korea [23456789]. The increase in diabetic patients also denotes an increase in the number of complications associated with diabetes. Diabetes is one of the top 5 causes of death in both developing and advanced countries including Korea; in Korea, diabetes ranked 5th in 2010 after cancer, cerebrovascular diseases, cardiovascular diseases, and suicide, whose prevalence increased by 5.6% since 2009 at a much faster rate compared with other diseases [10]. Diabetes patients usually die of stroke, myocardial infarction, etc., and complications such as amputation of feet, blindness, renal failure, etc., seriously dampens the patients' quality of life and add economic burdens due to treatments [11121314]. The cost for the management of diabetes is much higher than normal people, especially for diabetes-associated complications, presenting management of diabetes as an important personal and social problem [1516171819].
- The ultimate goal of diabetes management is to prevent complications by taking appropriate measures to improve diabetic patients' quality of life and reduce economic burdens from treatments. It has been reported that diabetes can be managed by proper regulation of blood glucose, blood pressure, dyslipidemia, etc. in order to reduce risks of complications [20212223]; thus, self-management by diabetic patients is of increasing importance with the help of guidelines for appropriate diabetes management and diabetes education [24252627]. In America, the Centers for Disease Control and prevention already recognizes the seriousness of diabetes and is continuing to check not only the prevalence of diabetes but also the diabetes-associated com-plications and the management status of diabetes, as well as running a prevention program [28]. However, not even the status of diabetes management is being systematically investigated in Korea, and the limited investigation that had been carried out only consists mainly of the data from health insurance and hospitals, revealing the lacking investigation state of diabetes management in Korea [29303132]. Furthermore, considering the importance of diabetes education and that diabetes education is mainly carried out in tertiary hospitals, it is necessary to determine exactly how diabetes management is being achieved in those tertiary hospitals.
- In this study we investigated the management status of type 2 diabetes patients in 13 tertiary hospitals in Seoul or Gyeonggi region. We intend to apply our data to provide a basis to develop diabetes management guidelines for individual medical institutions as well as utilizing it as base evidence to prepare appropriate plans for diabetes management in Korea. Identifying the standard of diabetes management and prevalence of diabetes-associated complications that could arise from it will be necessary for the preparation and establishment of national policies for diabetes that prepares for the immediate rapid increase in diabetes patients.
INTRODUCTION
- Study subjects
- Of the patients who visited the 13 randomly chosen tertiary hospitals in Seoul or Gyeonggi region for blood glucose control from 19th of March to 29th of May in 2013, 2,626 type 2 diabetes outpatients aged over 20 years that regularly visited these hospitals for more than 6 months for blood glucose control were investigated. Of these patients, 16 patients whose blood glucose control schedule did not match that of type 1 diabetes patients were excluded, and the final 2,610 patients were chosen for this study.
- During the investigation period, patients who matched this study's criteria were continuously recruited until a total of 100 patients were recruited from each hospital, and since the number of patients visiting each hospital was different, the registration dates were varied. This study was approved by the Institutional Review Board of each hospital with the same protocol.
- Study methods
- The details of the study subjects' demographical data, disease-related characteristics, blood test, prescribed medicine, associated diseases, and complications were gathered from their medical records. Medical records questionnaire was made and used based on both domestic and foreign treatment guidelines. To investigate the diabetes management status, the results of the blood glucose control indices, glycosylated hemoglobin (HbA1c); lipid; fasting glucose; 2-hour postprandial glucose; microalbuminuria; and ophthalmography tests, were collected. If no tests had been carried out during the previous 1 year, it was assumed that the tests were not performed.
- Diabetes complication was assumed only when it appeared in the medical records. Retinopathy was assumed if there was any abnormality in the test results, regardless of diagnosis. It was treated as 'no records' if the medical records had no history of any tests or diagnosis. The patients with albumin creatinine ratio of less than 30 µg/mg, microalbuminuria of 30 to 299 µg/mg, albuminuria of more than 300 µg/mg were regarded as normal for nephropathy, or 'no records' if they had no records. Renal complications were analyzed based on 8-hour, 24-hour microalbuminuria, albumin creatinine ratio, and medical records. The patients were assumed to have neurological complications if they were taking neuropathy medications or if they had previously been diagnosed with neurological complications, even if they were not diagnosed with any. They patients were assumed to have been educated for diabetes only if they had paid for and received one at a relevant center that provides the education at a fee; this was because the records of diabetes education from other centers were often missing and it is difficult to assess how well the patients were educated due to the varying standards of education from different centers. The patients were assumed to have other associated diseases only if any appeared in the medical records. In case of hypertension and dyslipidemia, the patients were assumed to have these disease if they were on antihypertensive or dyslipidemia drugs regardless of their diagnosis. All types of cancer were recorded. Fatty liver and liver cirrhosis were included in liver diseases, and both hyperthyroidism and hypothyroidism were included in thyroid diseases. The patients were analyzed after classifying them according to their diabetes treatment methods into diet therapy, insulin only, and combined insulin and oral hypoglycemic agent treatment, and drug history was investigated according to the patients' usage of hypotensive, cholesterol-lowering agent, and anticoagulant drugs.
- Blood glucose, blood pressure, and blood lipid modulation statuses were measured to assess the extent of metabolism control. The target value for adjustment was set as: <6.5% HbA1c, <130/80 mm Hg blood pressure, <100 mg/dL low density lipoprotein cholesterol (LDL-C), ≥50 and ≥40 mg/dL cholesterol in men and women respectively, and <150 mg/dL triglyceride as per the Korean Diabetes Association guidelines.
- Statistical analysis
- Statistical analyses were performed using the SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) with P values less than 0.05 being considered to have statistical significance. The frequency and percentage or the mean and standard deviation were obtained for all results. The general characteristics, the time of onset of diabetes, duration, blood glucose, blood pressure, and blood lipid levels that could differ depending on gender were analyzed by t-test. Family history, treatment method, experience of diabetes education, associated diseases, and complications that differed according to gender were analyzed by chi-square test.
METHODS
- The general characteristics of subjects
- The total of 2,610 study subjects consisted of 1,460 males (55.9%) and 1,150 females (44.1%). The average age was 61 years with 62.7 for females and 59.7 for males. The average body mass index (BMI) was 25 kg/m2 with 25.2 kg/m2 for females which was higher than the 24.9 kg/m2 of males (P=0.012). The average age at diagnosis of diabetes was 50.1±11.1 years, with the average female age (51.5 years) being higher than that of males (49 years). The duration was on average 10.7 years. In terms of family history, 955 patients (36.7%) had no records, and of the 1,646 whose record was available, 50.5% did have family history with no differences according to gender. For the treatment of diabetes, 71.6% only took oral hypoglycemic drugs, 17.3% took both oral hypoglycemic drugs and insulin, and 6.6% only took insulin; there were no differences according to gender. Of all subjects, 53.0% received education with a fee, and there were no differences in education frequency between males and females (Table 1).
- Associated diseases and diabetes complications
- Of the study subjects, 59.2% had hypertension with a higher proportion in males compared with females but with no statistical significance. For dyslipidemia, 65.5% of subjects were suffering from this disease, where the females had a higher proportion with 69.7% compared with 62.4% in males (P<0.001). The percentage of patients who had liver diseases was 18.3% with a higher proportion in females compared with males (P<0.001). The prevalence of tuberculosis and thyroid diseases were both 3.9%, with a higher prevalence in males for tuberculosis (P<0.001) but vice versa for thyroid diseases (P<0.001). Cancer was recorded in 8.9% of subjects consisting of 10.2% of males which was higher than the 7.2% of females (P=0.009) (Table 2).
- Diabetic retinopathy was present in 31.6% (641 patients) of the 2,030 who had medical records with no differences between males and females. Microalbuminuria test was performed in 73.3% (1,914 patients), and diabetic nephropathy was present in 28.1% (665 patients) of 2,363 patients with a higher percentage in males compared with females (29.9% and 25.9%, respectively; P=0.033). Microalbuminuria and macroalbuminuria was present in 18.7% and 11.2% of males and in 17.7% and 8.2% of females, respectively. Diabetic neuropathy was recorded in 19.9% of patients but there were no differences between males and females. Cerebrovascular diseases and cardiovascular diseases were present in 10.5% and 18.7% of patients, respectively, and a higher ratio of females had cardiovascular diseases compared with males (P=0.015) (Table 2).
- Level of metabolism control
- Medical record of systolic blood pressure was available for 2,587 patients showing an average of 125.4 mm Hg with a better regulation in females than males (P=0.026); both groups were being well controlled and within the normal range. HbA1c was tested in 99.8% of patients (2,606 patients) which showed that the average HbA1c was 7.3%±1.3% with no differences according to gender. Medical records of fasting glucose and 2-hour postprandial glucose were available for 2,223 patients (85.2%) and 1,744 patients (66.8%), respectively. The average fasting glucose was 137.2±45.0 mg/dL with no differences between males and females, and the average 2-hour postprandial glucose was 193.6±73.3 mg/dL with a higher ratio in males than females (198.0±71.5 and 187.9±75.1 mg/dL for males and females, respectively; P=0.004).
- The average total cholesterol was 163.3±36.5 mg/dL with a higher ratio in females (159.4±36.7 and 168.3±35.6 mg/dL in males and females, respectively; P=0.001), and the average triglyceride was 139.9±90.9 mg/dL with a higher ratio in males than females (144.9±103.4 and 133.4±70.9 mg/dL in males and females, respectively; P<0.002), The average high density lipoprotein cholesterol (HDL-C) was 49.5±14.2 mg/dL with a higher ratio in females (47.7±13.9 and 52.0±14.3 mg/dL for males and females, respectively; P<0.001), and the average LDL-C was 92.7±38.2 mg/dL which also had a higher ratio in females (90.5±30.7 and 95.6±46.1 mg/dL for males and females, respectively; P=0.002) (Table 3).
- Target achievement rate
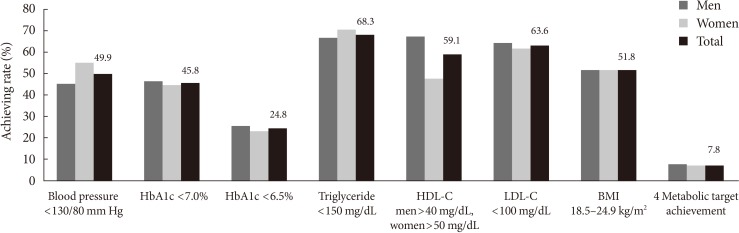
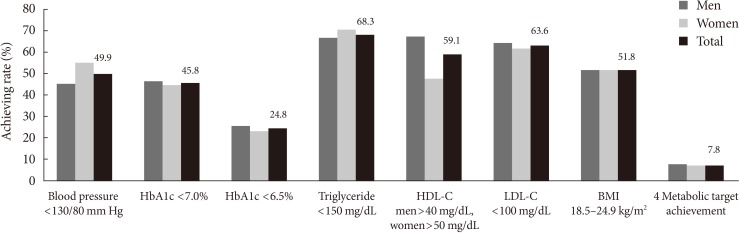
- The success rate of achieving the targets of <130/80 mm Hg, <7.0% HbA1c, and <6.5% HbA1c were 49.9%, 45.8%, and 24.8%, respectively. Reducing fasting glucose to <130 mg/dL and 2-hour postprandial glucose to <180 mg/dL was achieved in 51.5% and 48.6%, respectively. Total cholesterol and triglyceride was reduced to <200 and <150 mg/dL by 84.8% and 68.3%, respectively. Of all subjects, 68.3% maintained their HDL-C level to ≥40 mg/dL for males and ≥50 mg/dL for females, and 63.6% maintained their LDL-C to <100 mg/dL. The percentage of subjects with 18.5 to 24.9 kg/m2 BMI which is the normal range was 51.8% with no differences between males and females. Of all subjects, 14.5% (13.8% and 15.4% for males and females, respectively) reached all three target levels for blood glucose, blood pressure, and lipid level with no differences between males and females. The percentage of patients who successfully maintained all of blood glucose, blood pressure, lipid level, and weight management target levels was 7.8% (8.0% and 7.5% for males and females, respectively) with no differences between males and females (Fig. 1).
RESULTS
- This study investigated the status of diabetes management in 2,610 outpatients with type 2 diabetes from 13 tertiary hospitals in Korea based on the guidelines provided by the Korean Diabetes Association.
- Only 364 patients (14.5%; 13.8% of males and 15.4% of females) managed to reach the target values for blood pressure, blood glucose, and lipid level. Although this is higher than the averages of Asia (4.7%), developing countries (3.6%), and Europe (7.5%), it is lower than that of the United States (18.8%). Furthermore, the percentage of patients who succeeded in managing their blood pressure, blood glucose, lipid level, and weight was 7.8% (8.0% of males and 7.5% of females), which is lower than the average of Western countries despite the relatively lower rate of obesity, showing the necessity of a more active diabetes management. We also believe that this may be related to the fact that the people with abdominal obesity are more likely to have type 2 diabetes in Asia than in Western countries despite the lower BMI [26].
- The average HbA1c level in this study was 7.3%±1.3% without significant differences between gender, and 45.8% successfully regulated their HbA1c level to <7.0%. This percentage is higher than the 32.8% and 30.9% of the data from the Korean National Health and Nutrition Examination Surveys (KNHANES) and Health Insurance Data from 1998 and 2005, respectively, and it was also higher than the 30.9% and 36.7% of the study conducted in secondary and tertiary hospitals in 2001 and 2006, respectively [293032]. However, although the blood glucose control rate is higher than the average of the developing countries such as China, Eastern Europe, Asia, and Latin America, it remains lower than the United States, Europe, and Japan [3334].
- The prevalence of hypertension was 59.2% without significant differences between gender, and the rate of controlling blood pressure to <130/80 mm Hg was 49.9%, which is higher than the 36.4% of the average of developing countries, 15.8% to 37% higher than the KNHANES, and similar to 51.1% of the United States. Moreover, it was similar to the 43.2% and 66.3% from a study based on Korean tertiary hospitals [263132353637].
- The prevalence of dyslipidemia was 65.5% with a significantly higher prevalence in females compared with males. This percentage is far higher than the 14.1% from the National Health and Nutrition Survey performed in 2010, and also the prevalence of dyslipidemia in diabetic patients was higher compared with the 30% to 50% of other studies [293036]. We speculate this difference to be due to the average age of 61 years in this study which is higher than previous studies. The rate of controlling LDL-C to <100 mg/dL was 63.6%, which is higher than 25% to 50% of multiple other domestic and international studies [293136]. The lower rate of reaching the target for dyslipidemia in females evidences the sharp changes in female hormone after menopause, suggesting that dyslipidemia, a major cause for diabetes complications, should be thoroughly managed.
- The reason for the high control rate of blood pressure and LDL-C, despite the high average age and time from diagnosis of diabetes, is speculated to be due to the relatively high proportion of cardiovascular and cerebrovascular disease patients and the improved ability to adjust blood pressure and lipid level compared with the past. Nonetheless, since the major cause of death in diabetic patients is cardiovascular complications, a more thorough control of blood pressure and blood lipid is required.
- The average BMI in this study was 25.2±3.3 kg/m2 with a higher average in females compared with males, and this was similar to the 25.2 kg/m2 of diabetic patients in the National Health and Nutrition Survey in 2010 and the 25.0 kg/m2 of the article published by Lim et al. [30], and lower than Europe or the United States [29303839].
- The prevalence of retinal complications was 31.6% which is lower than the domestic tertiary hospitals, and the prevalence of renal complications was 28.1% which is similar to the 20% to 30% of previously reported studies. The prevalence of neural complications was 19.9% which is lower than a previous study which reported a prevalence of around 45% but higher than the 16.9% reported by tertiary hospitals. Except for retinal complications, these prevalences are lower than the averages of developing countries or Asia, while it is similar in part to the 24.5% prevalence of microvascular complications in Europe. We believe that the differences in the prevalence of neural complications, even between other domestic studies, is because of the wide variety of methods to diagnose neural complications and because of the improper diagnosis by several clinicians [2630313640].
- The prevalence of cardiovascular complications was 18.7% with no differences between gender, while that of cerebrovascular complications was 10.5% with a higher prevalence in males than females. In this study, postprandial glucose, systolic blood pressure, and triglyceride level were higher in males than females; although these differences could have led to the higher prevalence of cerebrovascular complications, we cannot be certain since no differences were observed in the rate of cardiovascular complications. The prevalence of cardiovascular and cerebrovascular diseases was higher than other domestic studies and the Asian average. This may be related to the average age and time from diagnosis of diabetes of our study subjects since the prevalence of macrovascular complications increases over time after getting diabetes [2630313639].
- As a method for treating diabetes, 71.6% only used oral hypoglycemic agents, similarly to previous domestic studies [145], 17.3% combined the usage of oral hypoglycemic agents and insulin, and 23.9% received insulin treatment which is similar to the 24.1% of studies by domestic tertiary hospitals and 15% to 25% of Europe but lower than the 30% of the United States. However, 6.6% only used insulin which higher than the 4.1% from the National Health and Nutrition Survey in 2005. This may be because this study was performed in a tertiary hospital and also related with the average age and time from diagnosis of diabetes of our study subjects [2931363839].
- Considering the speed at which the number of elderly population is increasing and that the age at which diabetes occurred was 50 years in our study, it is probable that the disease period of diabetes will also increase along with diabetes-related complications and become a social burden; hence, a more active treatment to control metabolism is required.
- The percentage of subjects who received education regarding diabetes at a cost was 53.0% which is similar to the 54.6% of the United States. However, this is higher than the national average of 40%; this difference is likely due to the fact that this study was conducted in tertiary hospitals within Seoul and Gyeonggi region. Nonetheless, further work should investigate the reason why sufficient education is not taking place even in hospitals with diabetes specialists. In this study, the level of education had no correlation with blood glucose control; we believe that this is because diabetes education only takes place once and blood glucose is managed without any further education for the rest of a patient's life. This shows the necessity of additional regular diabetes educations considering the characteristics of diabetes and the average time that a patient suffers from diabetes.
- Since our data was collected from only 13 different tertiary hospitals within Seoul and Gyeonggi region, it is difficult to announce that this represents the general management status of patients with type 2 diabetes. Therefore a further study with a larger cohort including diabetic patients from different medical centers over the country is needed and further continuous education and management is also required to keep blood glucose, blood pressure, lipid level, and weight within the target range. Hence caution is advised to prevent exaggerating the results of this study and generalizing it. A repeat study with prognostic data collection method is needed.
- In conclusion, the least well-managed between blood pressure, blood glucose, lipid level, and weight was blood glucose with more than 50% of subjects failing to reach the target. This represents the difficulty that patients are experiencing in regulating blood glucose which is the fundamental to diabetes management and shows that it requires more effort by the patients than hypertension and dyslipidemia which can be controlled by medication. Our results again stress the importance of diabetes education.
DISCUSSION
-
Acknowledgements
- This study was supported by a grant (K.H.S., 2012) from the Korean Diabetes Association.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
NOTES
- 1. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 2011;94:311-321. ArticlePubMed
- 2. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681-1688. ArticlePubMed
- 3. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129-2140. ArticlePubMed
- 4. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care 2009;32:2016-2020. PubMedPMC
- 5. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J 2011;35:303-308. ArticlePubMedPMC
- 6. Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes 2012;3:110-117. ArticlePubMedPMC
- 7. Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen CS, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G. 2010 China Noncommunicable Disease Surveillance Group. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948-959. ArticlePubMed
- 8. Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090-1101. ArticlePubMed
- 9. Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, Bhansali A, Joshi SR, Joshi PP, Yajnik CS, Dhandhania VK, Nath LM, Das AK, Rao PV, Madhu SV, Shukla DK, Kaur T, Priya M, Nirmal E, Parvathi SJ, Subhashini S, Subashini R, Ali MK, Mohan V. ICMR-INDIAB Collaborative Study Group. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia 2011;54:3022-3027. ArticlePubMedPDF
- 10. Statistisc Korea. Cause of death statistics 2012 updated 2013 Nov 25. Available from: http://kostat.go.kr/portal/korea/kor_nw/2/1/index.board?bmode=read&aSeq=308559.
- 11. Kim JH, Kim DJ, Jang HC, Choi SH. Epidemiology of micro- and macrovascular complications of type 2 diabetes in Korea. Diabetes Metab J 2011;35:571-577. ArticlePubMedPMC
- 12. Jin DC. Current status of dialysis therapy in Korea. Korean J Intern Med 2011;26:123-131. ArticlePubMedPMC
- 13. Ko SH, Cha BY. Diabetic peripheral neuropathy in type 2 diabetes mellitus in Korea. Diabetes Metab J 2012;36:6-12. ArticlePubMedPMC
- 14. van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B. The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil 2010;17(Suppl 1):S3-S8. ArticlePubMedPDF
- 15. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033-1046. ArticlePubMedPMCPDF
- 16. Lee KW. Costs of diabetes mellitus in Korea. Diabetes Metab J 2011;35:567-570. ArticlePubMedPMC
- 17. Kim TH, Chun KH, Kim HJ, Han SJ, Kim DJ, Kwak J, Kim YS, Woo JT, Park Y, Nam M, Baik SH, Ahn KJ, Lee KW. Direct medical costs for patients with type 2 diabetes and related complications: a prospective cohort study based on the Korean National Diabetes Program. J Korean Med Sci 2012;27:876-882. ArticlePubMedPMCPDF
- 18. Chang TJ, Jiang YD, Chang CH, Chung CH, Yu NC, Chuang LM. Accountability, utilization and providers for diabetes management in Taiwan, 2000-2009: an analysis of the National Health Insurance database. J Formos Med Assoc 2012;111:605-616. ArticlePubMed
- 19. Reutens AT, Atkins RC. Epidemiology of diabetic nephropathy. Contrib Nephrol 2011;170:1-7. ArticlePubMed
- 20. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580-591. ArticlePubMed
- 21. Stratton IM, Cull CA, Adler AI, Matthews DR, Neil HA, Holman RR. Additive effects of glycaemia and blood pressure exposure on risk of complications in type 2 diabetes: a prospective observational study (UKPDS 75). Diabetologia 2006;49:1761-1769. ArticlePubMedPDF
- 22. Shi L, Ye X, Lu M, Wu EQ, Sharma H, Thomason D, Fonseca VA. Clinical and economic benefits associated with the achievement of both HbA1c and LDL cholesterol goals in veterans with type 2 diabetes. Diabetes Care 2013;36:3297-3304. ArticlePubMedPMCPDF
- 23. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-2572. ArticlePubMed
- 24. Korean Diabetes Association. Treatment guideline for diabetes. 4th ed. Seoul: Gold Planning and Development; 2011. p. 40-129.
- 25. Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, Woo MH, Kim JY, Kim NH, Kim JT, Kim CH, Kim HJ, Jeong IK, Hong EK, Cho JH, Mok JO, Yoon KH. Committee of Clinical Practice Guidelines, Korean Diabetes Association. 2011 Clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J 2011;35:431-436. ArticlePubMedPMC
- 26. Chan JC, Gagliardino JJ, Baik SH, Chantelot JM, Ferreira SR, Hancu N, Ilkova H, Ramachandran A, Aschner P. IDMPS Investigators. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care 2009;32:227-233. PubMedPMC
- 27. Kim KS. Healthcare Benefit quality assessment of chronic disease. Health Insur Rev Assess Serv 2012;6:14-20.
- 28. Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med 2013;44(4 Suppl 4):S346-S351. PubMedPMC
- 29. Park SW, Kim DJ, Min KW, Baik SH, Choi KM, Park IB, Park JH, Son HS, Ahn CW, Oh JY, Lee J, Chung CH, Kim J, Kim H. Current status of diabetes management in Korea using National Health Insurance Database. J Korean Diabetes Assoc 2007;31:362-367.Article
- 30. Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: the committee of the Korean diabetes association on the epidemiology of diabetes mellitus. Korean Diabetes J 2009;33:48-57.Article
- 31. Lee YS. The current status of type 2 diabetes management at a university hospital. Korean Diabetes J 2009;33:241-250.
- 32. Kim SA, Park WS, Ohrr HC, Kang HY, Lee DH, Yi SW, Kwak YH, Song JS. Prevalence and management status of diabetes mellitus in Korea. Korean J Med 2005;68:10-17.
- 33. Guo XH, Yuan L, Lou QQ, Shen L, Sun ZL, Zhao F, Dai X, Huang J, Yang HY. Chinese Diabetes Education Status Survey Study Group. A nationwide survey of diabetes education, self-management and glycemic control in patients with type 2 diabetes in China. Chin Med J (Engl) 2012;125:4175-4180. PubMed
- 34. Pan C, Yang W, Jia W, Weng J, Tian H. Management of Chinese patients with type 2 diabetes, 1998-2006: the Diabcare-China surveys. Curr Med Res Opin 2009;25:39-45. ArticlePubMed
- 35. Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care 2013;36:2271-2279. ArticlePubMedPMCPDF
- 36. Lim DJ, Kwon HS, Kim HS, Lee JH, Ko SH, Lee JM, Kim SR, Lee WC, Son HS, Cha BY, Lee KW, Son HY, Kang SK, Yoon KH. Clinical characteristics of the diabetic patients managed at the different medical institutions in Seoul and Gyeonggi province. Korean J Med 2006;71:173-181.
- 37. Korean Diabetes Association. Diabetes fact sheet 2012 cited 2013 Sep 21. Available from: http://www.diabetes.or.kr/general/index.html.
- 38. Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med 2013;368:1613-1624. ArticlePubMed
- 39. de Pablos-Velasco P, Parhofer KG, Bradley C, Eschwege E, Gonder-Frederick L, Maheux P, Wood I, Simon D. Current level of glycaemic control and its associated factors in patients with type 2 diabetes across Europe: data from the PANORAMA study. Clin Endocrinol (Oxf) 2014;80:47-56. ArticlePubMed
- 40. Chuang LM, Tsai ST, Huang BY, Tai TY. Diabcare-Asia 1998 Study Group. The status of diabetes control in Asia: a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med 2002;19:978-985. ArticlePubMed
REFERENCES
Achieving rate in metabolic targets. Four metabolic target achievement: HbA1c <7.0%, Blood pressure <130/80 mm Hg, LDL-C <100 mg/dL, BMI 18.5 to 24.9 kg/m2. HbA1c, glycosylated hemoglobin; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; BMI, body mass index.
Clinical and disease-related characteristics
Comorbid diseases and diabetic complications (n=2,610)
Current level of metabolic parameters (n=2,610)
Figure & Data
References
Citations

- Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care
Tae Jung Oh, Jie-Eun Lee, Seok Kim, Sooyoung Yoo, Hak Chul Jang
CardioMetabolic Syndrome Journal.2021; 1(1): 88. CrossRef - Hypoglycemic efficacy and safety of Momordica charantia (bitter melon) in patients with type 2 diabetes mellitus
Soo Kyoung Kim, Jaehoon Jung, Jung Hwa Jung, NalAe Yoon, Sang Soo Kang, Gu Seob Roh, Jong Ryeal Hahm
Complementary Therapies in Medicine.2020; 52: 102524. CrossRef - Sociodemographic Factors Associated with Participation in Diabetes Education among Community-Dwelling Adults with Diabetes
Young-Hoon Lee
Yonsei Medical Journal.2020; 61(2): 169. CrossRef - Antidiabetic Effects of Vigna nakashimae Extract in Humans: A Preliminary Study
Soo Kyoung Kim, Jaehoon Jung, Jung Hwa Jung, Byong Won Lee, Sang Soo Kang, Gu Seob Roh, Jong Ryeal Hahm
The Journal of Alternative and Complementary Medicine.2018; 24(3): 249. CrossRef - Association of Self-Reported Dietary and Drug Compliance with Optimal Metabolic Control in Patients with Type 2 Diabetes: Clinic-Based Single-Center Study in a Developing Country
Thilak Priyantha Weerarathna, Miyuru Kavinda Weerarathna, Vidarsha Senadheera, Herath Mudiyanselage Meththananda Herath, Gayani Liyanage
Journal of Nutrition and Metabolism.2018; 2018: 1. CrossRef - A comparison of effects of DPP-4 inhibitor and SGLT2 inhibitor on lipid profile in patients with type 2 diabetes
Seon-Ah Cha, Yong-Moon Park, Jae-Seung Yun, Tae-Seok Lim, Ki-Ho Song, Ki-Dong Yoo, Yu-Bae Ahn, Seung-Hyun Ko
Lipids in Health and Disease.2017;[Epub] CrossRef - Effect of prescribing metformin according to eGFR instead of serum creatinine level: A study based on Korean National Health and Nutrition Examination Survey (KNHANES) 2009-2014
Sun Joon Moon, Chang Ho Ahn, Young Min Cho, Tatsuo Shimosawa
PLOS ONE.2017; 12(4): e0175334. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Features of Long-Standing Korean Type 2 Diabetes Mellitus Patients with Diabetic Retinopathy: A Study Based on Standardized Clinical Data
Sejeong Park, Sang Youl Rhee, Su Jin Jeong, Kiyoung Kim, Suk Chon, Seung-Young Yu, Jeong-Taek Woo
Diabetes & Metabolism Journal.2017; 41(5): 393. CrossRef - Influencing Factors of Knowledge, Attitude, and Practice regarding Medical Nutrition Therapy in Patients with Diabetes: A National Cross-Sectional Study in Urban China
Zijian Li, Haimin Jin, Wei Chen, Zilin Sun, Lulu Jing, Xiaohui Zhao, Sainan Zhu, Xiaohui Guo, China NEEDs Study Group
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Factors Associated with Participation in Diabetes Education: The Korea National Health and Nutrition Examination Survey 2007 to 2009
Jung Min Kim, Jae Won Hong, Jung Hyun Noh, Dong-Jun Kim
Diabetes & Metabolism Journal.2016; 40(6): 447. CrossRef - Health Performance and Challenges in Korea: a Review of the Global Burden of Disease Study 2013
Yo Han Lee, Seok-Jun Yoon, Arim Kim, Hyeyoung Seo, Seulki Ko
Journal of Korean Medical Science.2016; 31(Suppl 2): S114. CrossRef - Diabetic Cardiovascular Autonomic Neuropathy Predicts Recurrent Cardiovascular Diseases in Patients with Type 2 Diabetes
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Kyoungil Min, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko, James M Wright
PLOS ONE.2016; 11(10): e0164807. CrossRef
- Figure
- Related articles
-
- Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
- Change Profiles and Functional Targets of MicroRNAs in Type 2 Diabetes Mellitus Patients with Obesity
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis
- Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines

 KDA
KDA PubReader
PubReader Cite
Cite